Successful Diagnosis and Treatment of Occult Prostate Cancer Despite Multiple Negative Prostate Biopsies and Negative Prostate MRIs - Cancer Network
ABSTRACT
Prostate-specific antigen (PSA) values above 100 ng/mL often suggest metastatic prostate cancer. We present the case of a patient with a PSA of 110 ng/mL, 4 negative prostate biopsies, and 4 negative prostate MRIs. After his fifth MRI revealed a PI-RADS 5 lesion, he underwent his fifth transrectal biopsy; this revealed Gleason 3 + 4 = 7. He was found to have organ-confined pT2 disease on subsequent radical prostatectomy pathology. This case highlights that there may be no PSA for which one can assume metastatic disease with certainty. Depending on life expectancy, patients with extremely elevated PSA may still warrant a full staging workup
Introduction And Initial Presentation
A man, aged 73 years, presented to our care in early 2021 with a prostate-specific antigen (PSA) of 110 ng/mL after 4 negative prostate biopsies and 4 negative prostate MRIs. His journey had begun in 2002 when his PSA was 3 ng/mL. Two years later, in 2004, at a PSA level of 3.8 ng/mL, he had his first transrectal ultrasound-guided (TRUS) biopsy. All 6 cores were negative. His PSA continued to oscillate between 3 and 10 ng/mL for the next 5 years, warranting 12-core TRUS biopsies in 2007 and 2009. These were negative, and his prostate size of 40 grams was thus cited as the cause of his PSA elevation.
In 2010, as his PSA rose above 10 ng/mL, he had the first of 4 prostate MRIs; it did not reveal suspicious lesions. It was followed by a negative 12-core TRUS biopsy in 2011. His PSA rose from 65 ng/ml to about 100 ng/mL from 2014 to 2019, and repeat MRIs in 2014 and 2017 did not demonstrate any suspicious lesions. However, a mix of stromal and hyperplastic nodules in the transition zone (TZ) of the prostate were exhibited. Prostate MRI in 2019, at an outside academic center, again did not demonstrate a suspicious prostatic lesion. His prostate exam remained benign, with hypertrophy of the gland to
60 grams. In late 2020, his PSA measured above 100 ng/mL and he was referred to us for care.
Assessment
At presentation to our clinic in early 2021, the patient's PSA was 110 ng/mL, with minimal lower urinary tract symptoms and a negative review of systems. His prostate was 60 grams and smooth. An Exosome Dx urine test (EXO Dx; Exosome Diagnostics/Bio-Techne) revealed an extremely elevated score of 69 (normal is below 15.6). His Prostate Health Index (PHI; Beckman Coulter) was 259, and his percent free PSA was 7.5%. These prompted his fifth and final MRI.
Diagnosis And Management
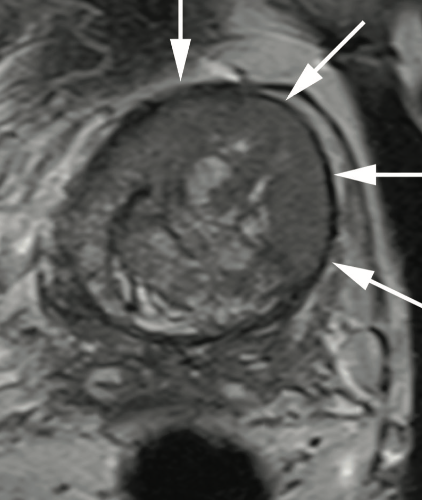
A PI-RADS 5 lesion was identified in the left anterior TZ (Figures 1A-1D), and an 18-core TRUS fusion biopsy shortly thereafter revealed 2 cores of Gleason 3 + 4 = 7, Gleason grade (GG) 2 disease (Figure 2A). After metastatic staging with a negative CT and nuclear medicine bone scan, he underwent open radical prostatectomy (RP) in May 2021. Final pathology revealed a 66-gram prostate, Gleason 4 + 3 = 7, GG3, organ-confined disease with negative lymph nodes, pT2N0Mx (Figure 2B).
Discussion
We used several novel secondary screening tests in this case: the PHI and the EXO Dx.1,2 Many contemporary patients are skeptical and reluctant to undergo an invasive prostate biopsy based only on total elevated PSA. Tutrone et al showed that compliance in following through on a biopsy using PSA alone was 39% vs 72% for men who also had an abnormal EXO Dx test to consider.3 Our patient was reluctant to have further invasive testing considering his prior negative work-up.
Although his high total PSA was outside the labeled indication for both tests, we felt the tests were useful in this most unusual case.
While infectious etiologies such as prostatitis, prostate abscess, and even tuberculosis can be considered, studies have shown that a PSA elevation due to an inflammatory prostatic process is often to a level much lower than what was seen with our patient.4 PSA values above 100 ng/ml do often suggest metastatic prostate cancer. In 1993, Stamey et al presented 3 similar patients with TZ lesions, PSA between 150 and 456 ng/mL, and Gleason 4 + 3 = 7: All were found to have organ-confined disease.5 TZ lesions have been shown to have higher PSA density than their peripheral zone (PZ) counterparts, and while large tumor volumes may be observed in the TZ, they are more likely to have favorable pathologic features and lower biochemical recurrence (BCR) rates.6 A more recent study in 2015 by Lee et al showed similar findings, with higher preoperative PSA values and larger tumor volume in TZ lesions compared with PZ lesions. Furthermore, they showed decreased odds of seminal vesicle invasion, extracapsular extension, and hazard of tumor recurrence.7 Additional study is needed to verify if the capsule around the TZ could be restricting tumor spread.
While a high PSA may be an excellent predictor, it is not perfect. A 2020 Swedish study of 8850 men with PSA above 100 ng/mL found that 71% had metastatic prostate cancer, and among men with PSA of above 500 ng/mL, the rate of metastases still ranged from 50% to 94%.8 Even if the disease is localized at the time of treatment, BCR is significantly higher for patients with PSA above 100 ng/mL who have undergone RP.9 BCR-free survival is only 29% at 10 years for PSA above 100 ng/mL for these patients.9
Q&A With Key Investigators
Q: Dr Moul, did you believe this patient had cancer when he presented to you? How did his past 4 MRIs and 4 biopsies impact your approach?
A: I do not recall seeing a prior patient with such a prolonged work-up and a PSA this elevated who did not have prostate cancer. When the PSA is above 100 ng/mL, the chance of finding prostate cancer is at least 75%.10
I am very fortunate to be at a major center with multidisciplinary care where we have access to secondary screening tests such as PHI and EXO Dx urine testing. When the EXO Dx returned at 69, I knew there was a high probability not only of cancer, but of Gleason 7 or higher. While the EXO Dx test is officially marketed for use in men with a total PSA between 2 and 10 ng/ml, I ordered the test to help convince this patient, who had already endured so much and felt well, to have another MRI and possibly another biopsy.3 Although the PHI is not approved for use in men with a total PSA of above 20, I also ordered this test, for similar reasons. In the end, we were able to identify what we believe to have been occult disease, and not interval cancer development, as anterior lesions can be missed in up to 46% of 12-core biopsies.11
Q: Dr Moul, had his repeat MRI not shown a lesion, what would your next step have been?
A: That is a great question. With total PSA, EXO Dx urine, free PSA, and PHI pointing to previously missed occult prostate cancer, I would likely have pushed the patient toward another biopsy. I would likely have recommended a saturation biopsy with special attention to anterior cores. The patient was understandably hesitant about more invasive testing and I believe it may have been challenging to convince him to do more testing, given that he felt perfectly fine. Fortunately, MRI did find the lesion that had been eluding his caregivers for [so long].
Q: Dr Moul, did you immediately consider surgery? What was your biggest concern in offering surgery?
A: I am very careful about offering RP to men 70 years and older due to concern for increased sexual and urinary morbidity in the group aged 70 to 79 years. However, this gentleman was enjoying excellent health and had a normal body mass index so I was a bit less concerned about incontinence. I did explain to him that age alone made him less likely to regain potency even with a bilateral nerve-sparing technique. I estimated his likelihood of regaining erections firm enough for intercourse, either spontaneously or with the help of oral medications, was about 20% to 25%. I also told him that he faced a 5% to 10% chance of still requiring a pad for stress incontinence at 1 year post surgery even though the risk of total incontinence was 1% or less in my series. Only RP pathologic assessment could help us understand why his cancer had been so elusive over the past 18 years. I did have the patient consult with radiation oncology as part of our multidisciplinary program and would have supported his decision for local therapy.12
Q: Dr Moul, what clinical pearls can we take away from this case from the perspective of a urologist?
A: Don't give up in healthy men who have elevated and rising PSA. This is an extreme and prolonged example of occult prostate cancer eluding multiple diagnostic and imaging efforts. I do not recall, in my 30-plus years of practice, ever seeing a patient with a PSA above 100 ng/mL who did not have prostate cancer. I think we were able to utilize the latest in technological advancements—those that did not exist 18 years ago when this patient first presented with an elevated PSA. Finally, this case had a happy ending with organ-confined disease on surgical pathology. No one would have presumed that this man with a PSA above 100 would have pT2 disease and at his 3-month follow up visit, the patient had a PSA less than 0.1 ng/mL and only mild stress incontinence (1 pad per 24 hours).
Q: Dr Gupta, what makes reading these MRI images so difficult?
A: Prostate MRI is a challenging imaging study to interpret, especially in the TZ. The TZ is challenging because of the overlap in imaging appearance of certain types of benign prostatic hyperplasia nodules with malignancy. Specifically, the degree of restricted diffusion and contrast enhancement can overlap with stromal and hyperplastic nodules, respectively. That said, there are morphologic features of anterior TZ lesions that are critical to recognize. Specifically, T2 weighted imaging is the dominant imaging sequence used to diagnose and characterize TZ lesions and these are characterized by an "erased charcoal" appearance, as in this case. Also, these lesions should have markedly restricted diffusion as evidenced by low signal on apparent diffusion coefficient (ADC) maps and high signal on high b-value diffusion weighted imaging (DWI).
Q: Dr Gupta, do you believe the 4 MRIs the patient had (2010, 2014, 2017, 2019) were all warranted? At what interval do you usually view meaningful changes in an MRI read?
A: This question really comes down to suspicion of clinically significant cancer. Clearly the patient had a PSA that was persistently elevated without imaging or biopsy findings to explain this. To that end, I think that repeat MRIs can be warranted. That said, it is critical to ensure high-quality MRI, with interpretation performed by radiologists with significant experience in prostate MRI. As for the interval during which we see meaningful changes on MRI, we can take some guidance from imaging performed as part of active surveillance protocols. In these cases, imaging can be helpful every 1 to 2 years, looking for changes in a lesion that would suggest that it is suspicious for clinically significant disease. This would include increase in size and/or increased restricted diffusion, as evidenced by lower signal on ADC maps and high signal on high b-value DWI.
Q: Dr Gupta, what imaging pearls can we take away from this case from a radiologist's perspective?
A: This case has some key takeaways. First, knowledge of the existence and prevalence of anterior TZ lesions is key to accurate diagnosis of these lesions. Radiologists are uniquely able to add value to patient care in this setting as these lesions are frequently missed on systematic biopsy due to their anterior location. Finally, when performing prostate MRI, even though PI-RADS states that decisions on lesion categorization should be made based on imaging findings only, in my opinion, prostate MRI cannot be read in a vacuum. That is, clinical information such as rising PSA must be considered when reading prostate MRI, especially when multiple exams have been performed.
Q: Dr Pendse, is there anything particular about this patient's tumor that ties together the PSA above 100 ng/mL and organ-confined disease?
A: High levels of total PSA have been shown to correlate with a larger volume of cancer, a high Gleason score (7 or higher), and capsular penetration in RP specimens.13,14 Also, the low percent free PSA levels were correlated with high Gleason score (7 or higher), and larger tumor volume. Our patient—with a very high total PSA level and a relatively low percent free PSA level of 7.5%, measured in 2021—had preoperative factors predicting a high Gleason score (7 or higher), larger tumor volume, and a higher chance of capsular penetration into the extraprostatic tissue. Additionally, the high PSA level also increased the preoperative probability of regional lymph node involvement.15
This case demonstrates that the accurate prediction of tumor burden and stage in a single individual can still prove to be tricky. As expected, the Gleason score was high at 4 + 3 = 7. Thenegative resection margins were surprising, though. A possible explanation for high PSA level and organ-confined disease may be the presence of significant disease burden in the anterior prostate. Higher PSA levels have been seen in anterior tumors. These tumors usually represent an extension of the more common posterior tumor and are often part of larger tumor foci.16 The tumor distribution in our patient with a high PSA involved the entirety of the left prostate including a significant amount of tumor in the anterior quadrant.
Q: Dr Pendse, can you describe the salient features of the pathology images (Figure 2)?
A: The RP specimen showed a dominant larger focus of prostatic acinar adenocarcinoma in the left prostate, extending from apex to base including both anterior and posterior quadrants (Figure 2B). The tumor showed a Gleason score of 4 + 3 = 7 with 70% pattern 4 and cribriform pattern 4. The striking feature on histopathology was the very compact arrangement of tumor cells compared with most cancer cases that I have seen, with very scant intervening stroma. I speculate that high tumor cell density contributed to the very high PSA level.
The final prostate biopsies showed prostatic adenocarcinoma in 5 of 18 cores. The lesion demonstrated on the MRI in the left anterior prostate showed prostatic adenocarcinoma 3 + 4 = 7, involving 7% of the tissue (Figure 2A; 100× magnification, hematoxylin and eosin stain). This finding of a much higher than expected tumor volume in the RP compared with prior biopsies is rather puzzling. Interestingly, Steiner et al have shown that in patients with repeat false negative biopsies, there is a statistically nonsignificant tendency toward a higher Gleason score and tumor stage in tumors detected via fourth or fifth biopsies compared with tumors detected via second set of biopsies.17
Q: Dr Pendse, what pearls can we take away from this case from a pathologist's perspective?
A: In a vast majority of cases, there is a high concordance level among tumor grade, volume, and distribution on biopsy and RP specimens. PSA levels are also correlative of tumor volume. In this patient, the tumor grade and volume were higher than expected based on multiple prior biopsies. The higher PSA level suggested a high tumor volume, which was confirmed on the prostatectomy. Organ-confined disease was somewhat unexpected. Every case is unique and can have surprising findings. Given their inherent uniqueness and profound implications on patient treatment and prognosis, it is important to practice with vigilance to not miss subtle diagnostic findings.
Conclusions
Ultimately, our case highlights that there may be no PSA for which one can assume metastatic disease with certainty and that using tumor location could help stratify patient risk. Depending on life expectancy, these patients may still warrant full staging workup. Considering the continuing controversy surrounding prostate cancer screening with PSA, some might argue that this is much ado about nothing.18 The patient was aged more than 70 years and clinically well. Ultimately, he had organ-confined disease that may have never seriously harmed him. In retrospect, this patient could have possibly lived his allotted life expectancy based on the fact that his disease was organ confined. However, we contend that the management was appropriate and justified and could have been a medicolegal risk if not addressed.
Author Affiliations:
Kostantinos E. Morris, BS1; Dominic c. Grimberg, MD1; rajan T. Gupta, MD1,2,3; avani a. Pendse, MD, PhD4; and Judd W. Moul, MD1,3
1Division of Urology, Department of Surgery, Duke Cancer Institute, Duke University Medical Center, Durham, NC
2Department of Radiology, Duke University Medical Center, Durham, NC
3DCI Center for Prostate and Urologic Cancers, Duke Cancer Institute, Duke University Medical Center, Durham, NC
4Department of Pathology, Duke University Medical Center, Durham, NC
Funding Support: This research received no outside funding
References
- Moul JW. Secondary screening tests for prostate cancer: is more information better? which test is best? Can J Urol. 2020;27(1):10086.
- Shore ND, Pieczonka CM, Henderson RJ, et al. A comparison of Prostate Health Index, total PSA, % free PSA, and proPSA in a contemporary US population--The MiCheck-01 prospective trial. Urol Oncol. 2020;38(8):683.e1-683.e10. doi:10.1016/j.urolonc.2020.03.011
- Tutrone R, Donovan MJ, Torkler P, et al. Clinical utility of the exosome based ExoDx Prostate (IntelliScore) EPI test in men presenting for initial biopsy with a PSA 2–10 ng/mL. Prostate Cancer Prostatic Dis. 2020;23(4):607-614. doi:10.1038/s41391-020-0237-z
- Morris KE, Grimberg D, Arcot R, Moul JW. Aggressive prostate cancer masquerading as acute prostatitis. Can J Urol. 2021;28(4):10799-10801.
- Stamey TA, Dietrick DD, Issa MM. Large, organ confined, impalpable transition zone prostate cancer: association with metastatic levels of prostate specific antigen. J Urol. 1993;149(3):510-515. doi:10.1016/s0022-5347(17)36131-1
- Erbersdobler A, Huhle S, Palisaar J, et al. Pathological and clinical characteristics of large prostate cancers predominantly located in the transition zone. Prostate Cancer Prostatic Dis. 2002;5(4):279-284. doi:10.1038/sj.pcan.4500602
- Lee JJ, Thomas I-C, Nolley R, Ferrari M, Brooks JD, Leppert JT. Biologic differences between peripheral and transition zone prostate cancer. Prostate. 2015;75(2):183-190. doi:10.1002/pros.22903
- Thomsen FB, Westerberg M, Garmo H, et al. Prediction of metastatic prostate cancer by prostate-specific antigen in combination with T stage and Gleason grade: nationwide, population-based register study. PLoS One. 2020;15(1):e0228447. doi:10.1371/journal.pone.0228447
- Tilki D, Mandel P, Karakiewicz PI, et al. The impact of very high initial PSA on oncological outcomes after radical prostatectomy for clinically localized prostate cancer. Urol Oncol. 2020;38(5):379-385. doi:10.1016/j.urolonc.2019.12.027
- Stattin K, Sandin F, Bratt O, Lambe M. The risk of distant metastases and cancer specific survival in men with serum prostate specific antigen values above 100 ng/ml. J Urol. 2015;194(6):1594-1600. doi:10.1016/j.juro.2015.07.082
- Ouzzane A, Renard-Penna R, Marliere F, et al. Magnetic resonance imaging targeted biopsy improves selection of patients considered for active surveillance for clinically low risk prostate cancer based on systematic biopsies. J Urol. 2015;194(2):350-356. doi:10.1016/j.juro.2015.02.2938
- Stewart SB, Bañez LL, Robertson CN, et al. Utilization trends at a multidisciplinary prostate cancer clinic: initial 5-year experience from the Duke Prostate Center. J Urol. 2012;187(1):103-108. doi:10.1016/j.juro.2011.09.040
- Horninger W, Rogatsch H, Reissigl A, et al. Correlation between preoperative predictors and pathologic features in radical prostatectomy specimens in PSA‐based screening. The Prostate. 1999;40(1):56-61. doi:10.1002/(sici)1097-0045(19990615)40:1<56::aid-pros7>3.0.co;2-e
- Partin AW, Yoo J, Carter HB, et al. The use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localized prostate cancer. J Urol. 1993;150(1):110-114. doi:10.1016/s0022-5347(17)35410-1
- Stamey TA, Kabalin JN, McNeal JE, et al. Prostate specific antigen in the diagnosis and treatment of adenocarcinoma of the prostate. II. radical prostatectomy treated patients. J Urol. 1989;141(5):1076-1083. doi:10.1016/s0022-5347(17)41175-x
- Vargas SO, Jiroutek M, D'Amico AV, Renshaw AA. Distribution of carcinoma in radical prostatectomy specimens in the era of serum prostate-specific antigen testing. implications for delivery of localized therapy. Am J Clin Pathol. 1999;112(3):373-376. doi:10.1093/ajcp/112.3.373
- Steiner H, Moser P, Hager M, et al. Clinical and pathologic features of prostate cancer detected after repeat false‐negative biopsy in a screening population. Prostate. 2004;58(3):277-282. doi:10.1002/pros.10330
- Mishra SC. A discussion on controversies and ethical dilemmas in prostate cancer screening. J Med Ethics. Published online July 6, 2020. doi:10.1136/medethics-2019-105979



Comments
Post a Comment