KEYNOTE-057 Results Add New Treatment Option for Certain ...
Physicians Discuss Up-Front Options For Unresectable Stage III NSCLC
During a Targeted Oncology™ Case-Based Roundtable™ event, Garrett B. Sherwood, MD, discussed options including concurrent chemoradiation therapy and neoadjuvant therapy for a patient with stage IIIA lung adenocarcinoma.
Garrett B. Sherwood, MD (Moderator)
Medical Oncologist
Novant Health Cancer Institute - Forsyth
Winston-Salem, NC
CASE SUMMARY
A 63-year-old man presented to his physician with intermittent cough and difficulty breathing on exertion. He had a history of hypothyroidism, which was managed on levothyroxine; and chronic obstructive pulmonary disease (COPD), which was managed on inhalers. He recently quit smoking and has a 40-pack-year history. His ECOG performance status was 1. Complete blood count, chemistries, and creatinine were within normal limits.
A chest CT scan showed a 3.1-cm spiculated left upper lobe (LUL) mass and 2 enlarged left mediastinal lymph nodes (stations 4L and 7), measuring 2.5 cm and 1.7 cm, as well as moderate emphysema. A PET scan confirmed lung lesion and mediastinal lymphadenopathy without evidence of distant metastases. His brain MRI was negative. Pulmonary function tests showed a forced expiratory volume of 1.2 and a diffusing capacity of the lungs for carbon monoxide of 35%.
Bronchoscopy with transbronchial lung biopsy of LUL mass and lymph node sampling via endobronchial ultrasound revealed adenocarcinoma at primary site, with positive nodes in stations 4L and 7. His cancer staging was T2aN2M0, stage IIIA.
DISCUSSION QUESTION
GARRETT B. SHERWOOD, MD: What do you think about the choice of biopsy? What would you do if this patient had no sufficient sampling from the lymph nodes at the time of bronchoscopy?
JONATHAN KRAUT, MD: Because of the location of the lymph nodes, navigational bronchoscopy or endobronchial ultrasound [EBUS] are completely suitable. It's been demonstrated by enough data that it is equal to a traditional mediastinoscopy. It's a reasonable approach. We would refer to the pulmonary department for an EBUS, traditional bronchoscopy, or even a navigational one.
SHERWOOD: If you're practicing in a situation where access to EBUS is limited or the primary care physician worked this up and did a CT-guided biopsy of the primary mass for lymph nodes that haven't been pathologically confirmed to be malignant, what criteria do you use to decide when to go back and recommend another biopsy? Or in the interest of simplifying the patient's evaluation, when to not send them back for another biopsy but just clinically stage them as stage III.
KRAUT: Mediastinoscopy is a great tool, and we still use it often. If they couldn't get to it with bronchoscopy, then traditional mediastinoscopy is a very useful tool to stage the patient.
SHERWOOD: What do you do in your practice if you happen upon a patient who you suspect has pathologic involvement of lymph nodes but that wasn't proven with their biopsy?
MAURIZIO BENDANDI, MD: This would be discussed in the tumor board…and maybe a collegial decision would be made. Sometimes patients have different outcomes based on the feelings of the group.
ARUN BHANDARI, MD: In our hospital, we have a multidisciplinary tumor board, and most of the EBUS and bronchoscopies are done by the thoracic surgeon, especially in such an area where it's stage III or stage II. Our thoracic surgeon will decide. They're pretty good with EBUS and bronchoscopy.
SUKHMANI GILL, MD: I work at Pardee Hospital in Hendersonville, [North Carolina], so we don't have our own thoracic surgeon, but we will send patients to Greenville [Memorial Hospital in South Carolina]. Our pulmonologists are good, but if they can't get to it, they will refer the patient. So by the time they come to me, we've already had this definitively handled. Even though we don't have our own thoracic surgeon, there is usually cohesive and good communication.
SHERWOOD: Great, thanks for sharing. As medical oncologists…we [usually] want more tissue for biomarker testing.
"What are the best up-front option(s) for this patient (some may include use of immune checkpoint inhibition)?"
DISCUSSION QUESTION:
SHERWOOD: I selected concurrent chemotherapy with radiation. I am very intrigued by some of the neoadjuvant chemoimmunotherapy data, and I believe they are going to be a paradigm-shifting option down the road. I want to see a little more of the [disease-free survival and overall survival] data mature. But as I work very closely with my surgical colleagues, I've learned that these cases do [have] an element of trickiness to them. Can someone who selected neoadjuvant chemoimmunotherapy talk us through their thought process?
BHANDARI: In the tumor board, it's a decision between the medical oncologist, radiation oncologist, and the surgeon. The surgeon can say, "I'm comfortable taking it out," or "I don't think it's resectable." Then concurrent chemoradiation is given. But it is a discussion had by the multidisciplinary tumor board. I picked neoadjuvant chemotherapy and immunotherapy because I'm confident the thoracic surgeon will probably agree with my opinion.
BENDANDI: I reluctantly picked neoadjuvant chemotherapy with or without immunotherapy, followed by surgery. I would say it should not be followed by surgery because the patient is deemed not to be a good surgical candidate. [At my hospital], we don't have [radiation therapy], so concurrent is rarely feasible. As for sequential, I hope that the future will be neoadjuvant chemotherapy plus immunotherapy, followed by surgery, [though] probably not in this case.
CHARLES KUZMA, MD: I don't think this patient has macroscopic N2 disease. That's usually not the ideal candidate for surgery. We identified that this patient, based on his pulmonary function, was never going to be a surgical candidate. For all those reasons, I chose concurrent chemoradiotherapy.
SHERWOOD: Those are all great points. N2 disease is a subgroup I'm going to be paying a lot of attention to when I'm looking at the CheckMate 816 study [NCT02998528]. There's a whole host of neoadjuvant immunotherapy alone and chemoimmunotherapy studies, which will be a lot for medical oncologists, surgeons, and radiation oncologists to sift through over the next few years.
KUZMA: I don't think a patient like this would have been eligible for CheckMate 816.
SHERWOOD: You're probably correct, based on those [pulmonary function tests]. I would imagine they would say that even if the patient had a complete response on imaging, that would be someone who would not do well with an operation. Dr Kraut, you're the only one here with experience operating after neoadjuvant chemoimmunotherapy. What's been your experience?
KRAUT: We've had very good outcomes with our patients. It's been a little more challenging in the interval from completion of treatment to surgery. Those patients have more desmoplastic changes, particularly around the lymph nodes, and the lymph nodes are around arteries and the bronchus. It's more [time] from a dissection standpoint, but it has not added a lot more time. If you look at some of the data that are out there, [it can be] anywhere between 30 to 45 minutes more due to the surgical complexity, but we've not [seen] that. Most of our patients have done very well. We [perform] them robotically; I think we've done all but 8 or 9 robotically. It's a little more complex because of the scarring and the desmoplastic changes, but overall, it's not been anything like when we used to see patients who had chemoradiation to the hilum.
SHERWOOD: Great, thanks for sharing.
CASE UPDATE
In this patient, the results of molecular testing show negative results for driver oncogenes in EGFR, ROS1, BRAF, ALK, RET, MET, ERBB2, NTRK, and KRAS. His PD-L1 expression level is 1%.
SHERWOOD: Does this change anyone's thoughts about what they would do for this patient? Not so much for me. I would probably still be recommending concurrent chemoradiotherapy.
BENDANDI: I would switch to chemotherapy plus sequential radiotherapy unless I can obtain it concomitantly. But the radiotherapy must be outside the VA [Veterans Affairs hospital].
SHERWOOD: Yes. I trained at a VA facility, and it was always a little problematic to refer someone outside the VA for radiation therapy, and to time concurrent chemotherapy with that, too. I recognize that conundrum.
Small Cell Vs. Non-small Cell Lung Cancer
Small cell and non-small cell are the two main types of lung cancer. There are several key differences, including the outlook for each.
In a person with small cell lung cancer, the cancerous cells appear small and round under a microscope. The cells of non-small cell lung cancer are larger.
Smoking is a major risk factor for both types. Of those who receive a diagnosis of small cell lung cancer, 95% have a history of smoking.
There are several subtypes of both small and non-small cell lung cancer. Non-small cell lung cancers include adenocarcinoma, squamous cell, and large cell carcinoma.
Small cell lung cancers vary depending on the expression of specific genes.
Some types are more aggressive than others, but generally, small cell lung cancer is more aggressive than non-small cell lung cancer.
Lung cancer — including both small and non-small cell types — is the third most common form of cancer among adults in the United States. Lung cancers account for 13% of new cancer diagnoses.
Small and non-small cell lung cancers cause similar symptoms. Sometimes, symptoms do not appear until the cancer reaches a later stage.
Symptoms include:
The symptoms of small and non-small cell lung cancers are similar, but small cell lung cancer spreads more rapidly.
A person may be more likely to experience symptoms after lung cancer has reached a later stage.
Does lung cancer affect women differently? Learn more here.
Can shoulder pain be a sign of lung cancer? Find out more.
Causes and risk factors for small and non-small cell lung cancer tend to be similar.
Smoking is the main risk factor. Cigarette smoke and the chemicals it contains can damage the lungs. This can lead to cellular changes that may result in cancer.
Additional risk factors include:
Smoking is a major risk factor for lung cancer. Find some ideas about how to quit here.
If a person sees a doctor about a persistent cough and other possible symptoms of lung cancer, the doctor will ask questions and take a medical history. They will also perform a physical examination.
If lung cancer may be present, the doctor will also request imaging scans, such as an X-ray or CT scan, and look for signs of a tumor, scarring, or a buildup of fluid.
They may also request samples of phlegm in order to perform a sputum test. This can help indicate whether cancer is present. The doctor will probably ask the person to provide a sample every morning for 3 days in a row.
Doctors may also perform a biopsy. This involves using a needle to take a sample of cells from the lungs for examination under a microscope. They may do this during surgery.
A biopsy can show:
Sometimes, the doctor requests a bronchoscopy. This procedure involves inserting a tool with a built-in camera through the mouth or nose and into the lungs. This helps them see the area and take tissue samples.
They may also carry out other tests to determine whether the cancer has spread beyond the lungs.
What does lung cancer look like? Find out here.
StagingThe stage of cancer describes how far it has spread within the body.
There are different ways to describe the stages. One simple way is:
However, each type of lung cancer has its own specific method of staging.
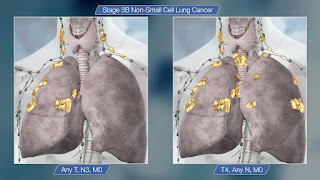
Non-small cell lung cancerFor this type of cancer, doctors typically use a 5-stage system.
Doctors generally categorize small cell lung cancer with one of two stages:
Some doctors use further staging for small cell lung cancer.
Can a person have both types?Around 5–28% of small cell lung cancer cases are "mixed." This means that the person has small and non-small cell lung cancers. Research suggests that it may be easier to treat mixed cancer than small cell lung cancer alone.
After making a diagnosis, a doctor will describe the treatment options and develop a treatment plan.
Factors that affect the plan will include:
As each person's situation is different, treatment will vary accordingly.
Non-small cell lung cancerTreatment options for non-small cell lung cancer include:
For small cell lung cancer, treatment mainly aims to manage the disease.
Options include:
Doctors may use a combination of treatments for lung cancer, depending upon an individual's needs, the stage of the cancer, and the location of the tumor.
Experts use past statistics to estimate the percentage of people who are likely to live for 5 or more years after a diagnosis of cancer. These estimations are called survival rates.
They represent averages and do not take into account factors such as a person's age or overall health.
Non-small cell lung cancerFor non-small cell lung cancer, the American Cancer Society (ACS) reports the following relative 5-year survival rates:
The overall average likelihood of living for at least another 5 years is 26%.
Small cell lung cancerThe ACS estimates the following 5-year survival rates for people with small cell lung cancer:
The overall average likelihood of living for at least another 5 years after a diagnosis of small cell lung cancer is 7%.
Other factors that may affect survival rates include whether the cancer has come back after treatment and a person's age. Recurring cancer and advanced age can have a negative effect on survival rates.
There are two main types of lung cancer: small cell and non-small cell. Small cell lung cancer is less common and more aggressive.
Quitting smoking — or never smoking — can significantly reduce the risk of developing any type of lung cancer.
Read this article in Spanish.
Mom, 37, With Stage 3 Breast Cancer Says Trying On Her Swimsuit Saved Her Life
As Julie Devaney Hogan put on her bikini over Labor Day weekend 2022, she felt a "barely there bump" below her nipple. Worried, she called her primary care doctor.
"I was told it was nothing to worry about," Devaney Hogan, 38, of Boston, tells TODAY.Com. "They said, 'Yeah, I wouldn't worry about it. You're scheduled for your physical at the end of October, just come in then.'"
 After noticing a lump in her breast below her nipple while putting on her bikini, Julie Devaney Hogan visited her doctor and eventually learned she had stage 3 breast cancer. She started Season for Squeezin' to encourage others to check out their breasts when wearing their swimwear.Courtesy Julie Devaney Hogan
After noticing a lump in her breast below her nipple while putting on her bikini, Julie Devaney Hogan visited her doctor and eventually learned she had stage 3 breast cancer. She started Season for Squeezin' to encourage others to check out their breasts when wearing their swimwear.Courtesy Julie Devaney Hogan Still, she scheduled an appointment with her OB-GYN and underwent tests, which revealed why she had a bump: It was stage 3 HER2 positive invasive ductal carcinoma breast cancer.
"My bikini saved my life," she says.
Lump leads to diagnosisAfter finding the "pea-sized" lump and being told by her doctor's office it was nothing to worry about, Devaney Hogan says she talked to her friends about it. One spoke up.
"My really good friend who's a nurse said, 'Absolutely not. Don't settle for not being seen,'" Devaney Hogan recalls. "She's like, 'I don't care what the doctor said. I don't care if they're not worried. Just get this checked. You have three babies — you need to be OK.'"
She called her OB-GYN in the hope she could be examined soon.
"Through a fair amount of pushing and persistence, I was able to get an appointment the following week," she says. "I probably could have pushed it off and been like, 'I'm busy, I've got stuff going on,' and I'm very grateful that I did it."
Her doctor referred her to a breast cancer facility, and she was again reassured that there was "nothing to worry about." She was told she could get a mammogram and biopsy, but she felt "there was zero urgency" in their recommendations. Still, she scheduled the tests.
"That bump was something. That bump was stage 3 HER2 positive and invasive breast cancer that had spread to my lymph nodes," Devaney Hogan says. "I very well could have brushed it off and waited. And I was told had I waited, we'd be in a very different scenario."
 Julie Devaney Hogan cutting a boob cake for her "boob voyage" party before her double mastectomy.Courtesy Julie Devaney Hogan
Julie Devaney Hogan cutting a boob cake for her "boob voyage" party before her double mastectomy.Courtesy Julie Devaney Hogan She underwent 12 rounds of chemotherapy, a double mastectomy, lymph node removal and radiation to treat her cancer. Recent scans found some residual cancer, so she started chemotherapy again, which will last until next year, and she will undergo reconstructive surgery in November.
When she was 35, Devaney Hogan actually had a mammogram because of recurrent mastitis in one breast. That made the diagnosis even more surprising.
"There were no other symptoms," she says. "I did not present in any way or have a family history or other symptoms that would put me at high alert."
Navigating motherhood, her career as a vice president at a tech company and cancer has felt tough at times.
"Cancer can somewhat be glamorized and dramatized on TV, so you have this expectation of what it's going to be, and suddenly I'm going to transition from a busy mother with a career to a very sick person," Devaney Hogan says. "The reality is you get the diagnosis and then you come home, and your kids are still yelling at you for not opening their string cheese the right way."
She took a leave of absence from work to focus on treatment and recovery.
"I really started to think of this as the new job in my life," she says. "I was going to be dedicating hours a week to ... Ensuring I got though this."
As she went through treatment, though, she pondered her diagnosis.
"You never expect it to be you. Maybe that's an awful thing to say," she says. "I feel great, and I exercise and eat well, and it's shocking."
 Julie Devaney Hogan hopes that Season for Squeezin' tags in swimsuits will encourage people to assess their breasts, even for those too young for mammograms.Courtesy Julie Devaney Hogan
Julie Devaney Hogan hopes that Season for Squeezin' tags in swimsuits will encourage people to assess their breasts, even for those too young for mammograms.Courtesy Julie Devaney Hogan She also felt like she knew her body well and wondered how she missed the lump.
"How was I so blindsided by the fact that this disease could get me," Devaney Hogan says. "That's where I started brewing this idea of squeezing and thinking about ways I could help ensure other women didn't have to think about breast cancer awareness only as a performative act ... In October."
Season for Squeezin'Prior to her diagnosis, Devaney Hogan thought about breast cancer awareness in October as an event that meant she needed to find pink clothes for her children to wear to school or raising awareness of an illness that impacted older women. She wondered if there was something she could do that could make breast cancer prevention more relevant to women under the recommended age for a mammogram. Season for Squeezin' was born.
"Unfortunately, breast cancer is impacting a growing number of younger women," she says. "Why not meet them and the place they are in the summer and focus on the things they can do really tangibly?"
Devaney Hogan reached out to swimsuit makers, asking to include tags with information about breast cancer detection and the Season for Squeezin' campaign. Heidi Fish — known for designing one of the bikinis Padma Lakshmi wore in Sports Illustrated — agreed to include the tags. Devaney Hogan recently learned that Imsy Swimwear and Kortni Jeane Swimwear will also use the tags.
Most medical groups no longer recommend routine self-breast exams as a way to screen for breast cancer because research hasn't found that they improve breast cancer detection or survival rates, according to Mayo Clinic. However, it is recommended to be familiar with your breasts so you can recognize changes and what's normal versus what's not — and take this information to a health care provider as soon as possible.
"We were founded to drive the message of giving yourself a squeeze each time you suit up in your swimwear," she says.
She's launching a campaign the week of June 18 to encourage people to take pictures of themselves in their swimsuits holding fruit and tag five of their friends to do the same — she hopes it reminds people to familiarize themselves with their breasts.
Since her diagnosis and starting Season for Squeezin', Devaney Hogan has learned a lot about herself. Throughout her career in the tech industry, others have told her to "tone it down" or be "demure" if she wanted to succeed. But she found that staying true to herself has made a huge difference.
"Being myself has saved my life. I was comfortable pushing for what I needed, speaking up and (leaning) into my ability to build relationships," she says. "It's terrible it takes a diagnosis like breast cancer to accept and celebrate who you are."




Comments
Post a Comment