Today' show star plans mastectomy and hysterectomy following ...
Surviving Lung Cancer Is Just The Beginning
More than 14,000 cases of lung cancer were diagnosed in Australia in 2022. Survival rates are the worst of all cancers, with just 22% surviving five years after diagnosis.
The best survival is seen in people with early-stage, localized disease—people who may not even feel unwell at the time of diagnosis. Australia is planning to introduce a National Lung Cancer Screening Program by July 2025, and so we expect to see many more lung cancers detected early, more people able to be treated with curative surgery and improvements in survival.
This is great news but it's just the first step. It is essential that we consider how we can maximize survivorship outcomes both now and in the future for people receiving lung cancer surgery.
Concerningly, a study recently found the prevalence of "functional limitations" in cancer survivors has rapidly risen over the last 20 years. Functional limitations are difficulties with physical activities like walking, standing up or carrying objects.
Very few people are limitation-free even years after treatment for cancer. Lung cancer survivors are the second most vulnerable (after pancreatic cancer)—with 76% reported living with functional limitations.
Cancer-related fatigue and breathlessness are also common and often continue long after surgery. This leads to a worsening pattern of difficulty moving, reduced fitness and muscle strength, and poor quality of life.
This comes with an associated economic burden as patients require extra care and other support like adapting their houses to accommodate their limitations.
The positive news for patients is exercise training has huge potential to address these limitations in people with lung cancer.
Strong research evidence has been produced over the last decade and we are now convinced that exercise is safe and highly effective in lung cancer therapy. We see consistent improvements in functional limitations, cancer symptoms, fitness, strength and quality of life for those who participate in an exercise program.
Surgery is the preferred treatment for people with early-stage lung cancer. This is usually delivered very close to diagnosis. In Australia, two-thirds of people undergo surgery within 14 days of a lung cancer diagnosis.
Fourteen days. Is that enough time to make a difference with exercise training before surgery? Our research published in the Cochrane Database of Systematic Reviews, in collaboration with Curtin University, suggests yes.
We found that exercise training results in a 55% reduction in the risk of lung complications after surgery. One extra person will be saved from a lung complication, like pneumonia, for every five people who exercise before surgery (compared to those not exercising).
Exercise programs as short as 14 days long are beneficial. People who exercise before surgery, compared to those who do not, stay in hospital shorter after their surgery and improve their fitness levels.
More research is needed to understand the long-term benefits of pre-surgery exercise and we are continuing to monitor patients after surgery to complete this picture.
Exercise training after surgery is also critically important and associated with excellent outcomes, including improved fitness, strength, breathlessness and quality of life. These exercise programs are longer, often six to 20 weeks in duration, as they are not restricted to the short timeframe before surgery.
The exercise programs are often delivered in a hospital gymnasium for a group of people with lung cancer. They usually run for 60 minutes and typically include aerobic exercises like stationary bike riding and treadmill walking, performed at a moderate "brisk" intensity. Other elements can include muscle strength training, balance exercises and stretches.
The strength of evidence now challenges us to consider how all Australians living with lung cancer can be supported to exercise.
People with lung cancer have significant barriers to exercise and we cannot expect most people to exercise without the support of health professionals. The exercise programs that we know work—because they have been tested in clinical trials—are supervised by health professionals, mostly physiotherapists.
It is important for patients to be screened for safety and given a careful, tailored exercise prescription. Yet despite the complexity of care required, we found that in Australia there are very few exercise programs available for people with lung cancer.
This is partly because we have only gathered the evidence to understand the efficacy of exercise for lung cancer in recent years and clinical practice has not yet caught up.
Similar exercise programs are already well established nationally and internationally for other conditions, including hospital or community-based Pulmonary Rehabilitation. The evidence supporting exercise for people with chronic obstructive pulmonary disease "COPD' was initially generated decades ago.
Many of the pulmonary rehabilitation programs have now expanded to include people with "other" respiratory diseases like lung cancer. However, demand is very high and waitlists are long.
Our team are currently trialing a remotely delivered exercise program, using physiotherapy support through weekly phone calls for 12 weeks after lung cancer surgery. The trial was outlined in a preliminary article published in BMJ Open Respiratory Research.
Whether or not such a hands-off home-based program can achieve the same magnitude of patient gains is the big question we hope to answer.
Certainly, the exercise program is less resource intensive for patients as they don't need to travel to a hospital gymnasium to see the physiotherapist and exercise. If shown to be effective, the program could be scaled up nationally in time for the introduction of the National Lung Cancer Screening Program.
There are promising times ahead for the management of lung cancer. We are finally at a point where we truly understand the benefits, and safety, of exercise.
For many people, exercise is a positive activity, that they can control, in an otherwise terrible time in their lives.
More information: Preoperative exercise training for people with non-small cell lung cancer, Cochrane Database of Systematic Reviews (2022). DOI: 10.1002/14651858.CD012020.Pub3
Catherine L Granger et al, Effect of a postoperative home-based exercise and self-management programme on physical function in people with lung cancer (CAPACITY): protocol for a randomised controlled trial, BMJ Open Respiratory Research (2022). DOI: 10.1136/bmjresp-2021-001189
Citation: Surviving lung cancer is just the beginning (2023, July 31) retrieved 31 July 2023 from https://medicalxpress.Com/news/2023-07-surviving-lung-cancer.Html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without the written permission. The content is provided for information purposes only.
VA's Small Steps Are Leading To A Giant Step Toward Surviving Cancer
One in three Americans will be diagnosed with cancer in their lifetime. While the health care system has made incredible advances, far too many people still feel cancer's devastating impact.
In early 2022, President Joe Biden and First Lady Jill Biden re-ignited the Cancer Moonshot to reinvigorate national action to defeat cancer, with the goal to reduce cancer deaths by 50% in the next 25 years.
The Department of Veterans Affairs has been at the forefront of the Cancer Moonshot as a member of the president's Cancer Cabinet, and as the largest integrated provider of health care and cancer care nationwide. The VA serves about 9 million enrolled veterans at more than 1,300 health care facilities, including treating roughly 43,000 veterans for cancer every year.
To meet the Moonshot challenge, VA is boosting screening and virtual treatment options, leveraging technology and innovative therapies, and offering veterans access to new clinical trials. We are focused on reducing four major groups of cancer most diagnosed within the veteran population: lung, colorectal, prostate and bladder.
Lung cancer, for example, is the second most common type of cancer and is by far the leading cause of cancer death within the veteran community, taking approximately 5,000 veteran lives every year.
Early detection saves livesAccording to the American Lung Association, nearly half of all lung cancer cases in the U.S. Are diagnosed at a late stage when the survival rate is only about 6%. The survival rate goes up to about 60% if diagnosed at an early stage. Consistent and routine screening is essential to the estimated 1-2 million veterans at risk for lung cancer.
High-quality, accessible screening is a cornerstone of VA's cancer care. In fact, in 2022, VA was recognized with a FedHealth IT Innovation Award for work by its National Center for Lung Cancer Screening to increase the number of eligible veterans getting screened for lung cancer.
VA's National Center for Lung Cancer Screening has worked to provide systematic, integrated, and high-quality screening. The center recently implemented an electronic health record alert at over 100 VA medical centers that provide lung cancer screening. These electronic alerts have become part of the system of care and have resulted in VA increasing the number of veterans screened for lung cancer by 560% compared to pre-pandemic screening rates.
During a Cancer Cabinet Community Conversation hosted by VA as part of the Cancer Cabinet, lung cancer survivor and U.S. Air Force veteran Brian Sturgill urged veterans to ask their provider about lung cancer screening and find out if they qualify. Sturgill, whose lung cancer was already metastatic when first diagnosed, is a survivor, but only after he underwent surgery to remove a section of his small bowel and a lobe of his lung.
"If we had screening 12 years ago, I don't know if I would have needed a small bowel resection," said Mr. Sturgill. Now well into his survivorship journey, Mr. Sturgill is a lung cancer clinical trial coordinator. His personal experience with clinical trials, lung cancer, and survivorship serves as a model for veterans and the importance of lung cancer screening.
Where you live shouldn't determine whether you surviveThere are more than 2.7 million veterans enrolled in VA who live in rural and highly rural areas, many with no cancer specialists near their homes. VA is addressing this need through the creation and expansion of VA National TeleOncology, bringing sub-specialized cancer care to veterans in locations across the nation, with more than 55 sites currently active and more on the way, access to VA's virtual cancer care continues to grow.
Multidisciplinary teams will provide expert sub-specialized oncology services as well as care coordination across the cancer care continuum, from diagnosis to survivorship or palliative care. Through VA's recently launched Virtual Tumor Board, disease-specific experts lend their support for complex cases and rare cancers as well across the enterprise.
Clinical trials and the future of cancer careThe National Cancer Institute has partnered with the VA to enroll veterans with cancer — especially from underrepresented populations. As of 2021, 25% of patients enrolled in these trials were from minority populations.
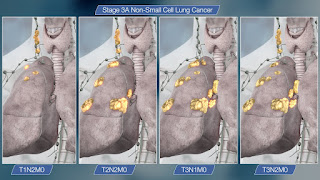
We have created the Enhance Equity and Access to Clinical Trials, or ENACT, program that will add to existing programs and infrastructure while developing innovative strategies to help veterans and VA oncologists connect with clinical trials. This also means finding connections to clinical trials not traditionally used. For example, we have observed that there is a substantial improvement in survival over time that corresponds to the timing of approval of targeted therapy, particularly for non-small cell lung cancer.
A relentless commitmentVA has been a pioneer in the field of research, specifically cancer research. In 1933, Robert Schrek, a leader in the field of radiosensitivity, identified the first connection between sun exposure and skin cancer while at the Tumor Research Laboratory at the Hines VA Hospital in suburban Chicago. Longtime VA scientist Dr. Ludwig Gross was one of the great pioneers of cancer research and the father of modern retrovirology. During the years of the original race to the moon — the 1950s and 1960s — Gross was conducting laboratory studies on mice that eventually proved that leukemia in mice was caused by a virus.
The Cancer Moonshot has refocused VA's efforts on cancer, working to end cancer mortality as we know it. And VA is working to improve access for veterans at every step in their cancer care journey and helping veterans and their families take that giant leap to survival. To learn more about cancer care at VA, visit Cancer.VA.Gov.
Dr. Carolyn Clancy is the Veterans Health Affairs assistant under secretary for health for discovery, education and affiliate networks. Dr. Michael Kelley is the VA National Oncology Program executive director.
Have an opinion?This article is an Op-Ed and as such, the opinions expressed are those of the author. If you would like to respond, or have an editorial of your own you would like to submit, please email us. Want more perspectives like this sent straight to you? Subscribe to get our Commentary & Opinion newsletter once a week.
Share:
Little-known Sign Of Deadly Lung Cancer Can Be Spotted At Nail Salon - What To Look For
One of the symptoms of serious health issues like lung cancer is finger clubbing, a medical condition that changes the shape and appearance of fingers, fingernails, and toes
Finger clubbing causes changes in finger shape and appearance due to underlying conditions (Image: Getty Images/iStockphoto)
Nail salons could be unlikely allies in the fight against deadly lung conditions, with medical experts urging patients to be vigilant for a little-known but significant symptom known as "finger clubbing."
Beyond the allure of perfectly manicured nails lies a potentially life-saving clue that could signal the presence of severe underlying health issues, including fatal lung cancers.
This seemingly innocuous sign, characterised by subtle changes in the shape of fingers and fingernails, has caught the attention of the medical community, prompting a call for heightened awareness and early detection.
Consult a doctor if you spot this distinctive phenomenon during your next visit to the nail salon.
Uncovering the hidden link between nail health and respiratory well-being might just be the key to saving lives in the battle against these stealthy diseases.
It affects fingertips and sometimes toes, developing in stages over several years (Image:
Getty Images/iStockphoto) What is finger clubbing?According to Cancer Research UK, finger clubbing, also known as digital clubbing or Hippocratic fingers, is a medical condition characterised by specific changes in the shape and appearance of the fingers and fingernails.
It typically affects the fingertips of both hands and in some cases, the toes as well. The development of finger clubbing occurs in stages and is associated with various underlying health conditions, particularly those related to the lungs or heart.
The stages of finger clubbing include:
Image:
Getty Images/iStockphoto) What causes finger clubbing?One of the possible causes is the presence of large cells called megakaryocytes getting trapped in the small blood vessels in the fingertips, leading to increased blood vessel and tissue growth, as well as fluid buildup.
Finger clubbing typically develops gradually over a period of years, but in certain conditions like a lung abscess, it may progress more rapidly.
Other symptoms of lung cancerLung cancer can present with various symptoms, although some individuals with early-stage lung cancer may not experience noticeable symptoms. As the cancer progresses, common symptoms of lung cancer may include:
However, these symptoms can also be associated with other conditions, and do not necessarily mean a person has lung cancer. If you experience any of these symptoms, especially if they persist or worsen over time, consult a healthcare professional for evaluation and appropriate testing.
The condition may result from trapped megakaryocytes and increased blood vessel growth (Image:
Getty Images/iStockphoto) What can you do if you spot finger clubbing?If you notice finger clubbing or any other concerning symptoms, it's essential to schedule an appointment with your doctor or a healthcare professional for a thorough evaluation.
During the appointment, the doctor will conduct a physical examination, inquire about your medical history and any other symptoms you might be experiencing. They may also order further tests to investigate the underlying cause of the finger clubbing.
Depending on the findings, your doctor may recommend specific tests, such as a chest X-ray or other imaging studies to assess the condition of your lungs and heart.
These tests can help identify potential underlying causes, including lung cancer or other related conditions.
It's essential not to self-diagnose or ignore the symptoms, as finger clubbing can be a sign of various serious health conditions.
Early detection and proper medical evaluation can lead to timely intervention and treatment, which can significantly improve outcomes for any underlying health issues.




Comments
Post a Comment