Colon Cancer and Back Pain: Symptoms, Causes, Treatments
Oncology/Cancer: 2023 Advancements And Breakthroughs
When one thinks of the most wide-reaching, deadly health issues facing the world today, cancer has to be right up there at the top of the list.
The wide range of diseases encompassed by the disease affect people of all walks of life in all corners of the globe.
In the United States alone, recent figures show there were an estimated 1.9 million new diagnosed cases of cancer in 2022 along with 609,360 cancer deaths.
Zooming out for a more global perspective, cancer stands as the second most common cause of death worldwide, accounting for almost 10 million deaths in 2018, the World Health Organization (WHO) reports. That was nearly one in every six deaths.
The World Cancer Research Fund International states that there were 18 million cancer cases globally in 2020. About 9.5 million were reported in men while 8.5 million were seen in women.
Given these statistics, where are we today in the push to develop new treatments?
The research now out there is offering us a more comprehensive understanding of how cancers are affecting millions of people around the world.
Healthline spoke with some experts to contextualize the big breakthroughs in oncology research and treatment over the past year as well as predictions of what we should be looking in the year ahead.
Experts say that mRNA technology has yielded exciting results
Throughout this year, news was made regarding various clinical trials for potential cancer therapies that were developed by way of mRNA technology, which was used to develop the COVID-19 vaccines.
MRNA refers to a kind of nucleic acid, which essentially communicates ways the body can produce needed proteins. When mRNA is injected into the body via a vaccine, for instance, it communicates with the body's cells to trigger an immune response to the kinds of abnormal proteins created by a cancer, according to the National Cancer Institute.
A range of trials are testing whether the success seen with COVID-19 can work with cancers.
A team from Memorial Sloan Kettering Cancer Center in New York funded by the National Institutes of Health (NIH) has been developing an mRNA vaccine for pancreatic cancer.
In this small study, customized vaccines were engineered successfully for 18 of the 19 participants.
Throughout the study, 16 remained at a healthy threshold to receive some of the vaccine doses and half of them saw the vaccine trigger T cells needed to target their pancreatic cancer.
The results were encouraging, but a mixed bag — after a year-and-a-half post-treatment period, those who had a strong T cell response did not show signs of the cancer returning. The other half who didn't respond to the vaccines with T cell activation saw their cancer return within an average of one year, reports NIH Research Matters.
Dr. Janice Mehnert, a melanoma expert and medical director of NYU Perlmutter Cancer Center's Clinical Trials Office in New York, told Healthline that the Moderna mRNA vaccine program is currently "a super exciting space to watch."
The drug manufacturer has been engaging in promising mRNA vaccine clinical trials in non-small cell lung cancer, for which it's partnering with Merck on a phase III trial, as well as two vaccine trials for melanoma.
In July, the companies announced a phase III trial of a combination therapy that consists of mRNA-4157 plus pembrolizumab, brand name Keytruda, for people who are at high risk and who've received surgery. The goal is to enroll 1,089 people at melanoma stages IIb to IV, with final trial results expected in 2029.
Earlier in the year, the two companies reported results from a phase 2b trial of mRNA-4157 and pembrolizumab in a 157-participant trial. It revealed a 44% decrease in risk of post-surgical melanoma recurrence or death, compared to the risk with pembrolizumab used on its own. This combination therapy has earned breakthrough designation from the U.S. Food and Drug Administration (FDA).
Mehnert said that these developments combine "two of the most exciting breakthroughs in medicine — mRNA vaccine technology and immunotherapy in a personalized tumor informed approach."
There was also news about antibody drug conjugates (ADCs)
"Antibody drug conjugates are a major space to watch with huge breakthroughs in breast and bladder cancer as well as lung and stomach cancer," Mehnert said.
What are they?
Antibody drug conjugates (ADCs) are basically a way to directly target cancer cells without causing the toxic damage of chemotherapy. They consist of monoclonal antibodies attached to the drug itself by way of a linking chemical that can directly hit the cancer cells in question.
The journal Frontiers in Immunology reports that ADCs have proven successful in preclinical and clinical trials, and some have even been approved by the FDA to treat some types of cancer. It's a growing field and 2023 saw it continue to be high on everyone's radars.
Given how the disease presents itself so differently between individuals and the many forms it takes, cancer is one of the more complex health issues that frustrates clinicians and patients alike.
Samuel Godfrey, PhD, a research information lead at Cancer Research UK, said that is changing partially due to the work of TRACERx, a project that aims to deliver "the most detailed understanding of cancer evolution ever."
"We learned how cancer's capacity for rapid change is inexhaustible, which helps explain why this disease is such a challenge to beat. TRACERx has showed that it is actually possible to spot patterns and predict cancer's behavior, even among such high levels of complexity. Realistically we could one day predict how a cancer progresses and perhaps even intervene before it becomes a problem," Godfrey told Healthline.
Mehnert added that the advent of novel bispecific T cell engagers marks another big 2023 cancer development.
These are artificial antibodies that essentially aim a person's T cells to their intended cancer cell target.
"They can redirect the entire repertoire of T cells against tumor, independent of T-cell receptor specificity," according to the BMJ Journal for ImmunoTherapy of Cancer.
Godfrey also pointed to clinical trials such FOxTROT from the University of Birmingham in the United Kingdom and INTERLACE out of University College London as showing great promise in "markedly improved cancer survival."
"What I find exciting about these trials is that the breakthroughs weren't about new, expensive medicines but rather using well-established, cheaper drugs," he said. "In short, with treatment, it might be all about timing."
Many of the advancements and breakthroughs these experts cited are currently in trials, some of them might be years away from making a direct, concrete impact in cancer care.
Some of them are already changing the game.
It's a wide range, just in the same way cancers themselves affect people around the globe in such broad and varied ways.
When asked what he sees on the horizon, Godfrey said that now is a time of "much optimism and excitement in the science community."
"As we look forward to 2024, I am particularly excited about seeing many small but vital steps toward better prevention, diagnosis and treatment," he added. "I think there will be further innovation in the use of our own immune systems to tackle cancer. We'll see more improvements to technology that can detect the earliest signs of cancer. And AI [artificial intelligence] will continue to allow our scientists to do more, taking on some of the toughest cancer challenges such as predicting who is most at risk of the disease."
"There is still a long way to go, but it is very inspiring to see how we are steadily moving toward a future where cancer won't be a major problem," Godfrey said.
I Was 28, Healthy And Fit When A Routine Blood Test Led To A Stage-four Cancer Diagnosis: Then They Gave Me Three Years To Live
Samantha Bulloch went from enjoying her 20s to having as little as three years left to live after doctors found life-threatening tumours spread through her colon, liver and right lung following a routine blood test.
On February 28, the healthy and fit library assistant had her world turned upside down after being diagnosed with stage four colorectal cancer that had spread to her organs.
In January, Samantha, from Sydney, visited her GP for a blood test to check her iron which led to the detection of the cancer.
'I don't drink, I don't smoke, I'm not overweight, I don't eat processed meat, I barely eat red meat, and have no family history of bowel cancer - it just didn't make sense,' Samantha, now 29, told FEMAIL.
Her symptoms included 'random' fatigue, the odd bout of bloating and some blood spotting during 2020 which she put down to stress. Before her test she also had some severe pain in her shoulder.
At this stage she'll remain on fortnightly treatment indefinitely. If the cancer remained undetected she believes doctors would've had few options for her moving forward.
Samantha Bulloch went from enjoying her late 20s to having as little as three years left to live after doctors found life-threatening tumours spread through her colon, liver and right lung after a routine blood test
'I don't drink, I don't smoke, I'm not overweight, I don't eat processed meat, I barely eat red meat, and have no family history of bowel cancer - it just didn't make sense,' Samantha, now 29, told FEMAIL
'I thought I was fit and healthy! I've always had iron problems but never thought too much of it. One day at work I was way more tired than normal and I had to sit down because I was so exhausted,' she said.
'I thought "that's weird" but assumed it was because I had started a new job, had low iron and was learning the ropes of something completely different. It was close to Christmas too and everyone is always tired by the end of the year.'
So she made the responsible decision to go see her doctor in January 2023.
The blood test results confirmed she's anaemic but also highlighted something unexpected - her liver enzymes were 'three times outside the normal rate'.
The GP made an appointment to do an ultrasound on Samantha's liver which revealed 'non-specific lesions' and a mass. The report also listed a variety of illnesses that it could be - one of them being cancer.
'When I saw that I already thought it was a death sentence,' she said.
A week later the results from a CT scan confirmed Samantha's worst fears - she had a tumour growing in her sigmoid colon which had spread to her liver and right lung.
A blood test confirmed she's anaemic but the results also highlighted something unexpected - her liver enzymes were 'three times outside the normal rate'
'I thought how have I been living with tumours growing in my body and didn't know about it? It was wild to me,' she said.
'I remember sitting in that appointment with my GP and my dad thinking "it's over, they're going to tell me there's nothing they can do".
'I knew how bad it was and that absolutely terrified me.'
The tumour in her colon was 6cm, the two in her liver were 8cm and the one in her right lung was 1.5cm. She also has a 'bunch of little tumours' scattered in her liver that can't be measured.
The life-changing news shook Samantha to her core and at first she initially thought, 'I can't do this, I don't want to do this, I'm not strong enough to do this'.
'I didn't even want to attempt it but somehow I put on my big girl pants and took myself to the next appointment. The first few months were so up and down emotionally - I couldn't stop crying on the first day of treatment.'
The tumour in her colon was 6cm, the two tumours in her liver were 8cm and the one in her right lung was 1.5cm. She also has a 'bunch of little tumours' scattered in her liver that can't be measured
Samantha said in 2020 she had a small amount of bleeding during bowel movements - but didn't think it was anything of concern. At the time it was the start of the pandemic, so seeing a doctor was difficult.
'It was on and off for a couple months, and when it finally resolved itself I forgot about it,' she said.
By the end of 2022 she did say she experienced some pain, bloating and irregular bowel movements. These symptoms are commonly brushed off as stress.
'At the start of this year I also had the worst pain in my right shoulder - it was excruciating, I was in tears. I went to the doctor who told me to take some Panadol because I may have just pulled a muscle,' she said.
The pain went away after a week or so, but strangely enough, it turns out the pain was due to the tumours in her liver.
'After I had my first liver biopsy, the pain in my right shoulder returned and the doctor told me that can happen because there's a nerve that sits right where your liver is,' she explained.
'So if that nerve gets pushed on by something it aggravates the nerve and you feel the pain in your right shoulder, which made it so much sense.'
Luckily after starting chemotherapy treatment in March, all the tumours have shrunk in size (pictured with friends)
Two days after the diagnosis she met with an oncologist and 'barely remembers the conversation' because of the hefty life-changing news and bawled her eyes out.
But the oncologist had a plan of attack.
Instead of having surgery first, doctors opted to go with chemotherapy in attempt to shrink the tumours.
Samantha started treatment on March 31 and she's been having fortnightly visits ever since. By her sixth chemotherapy session the tumours had shrunk significantly.
Her last scan at the beginning of October found the colon tumour had 'collapsed' - meaning it's flattened against the wall of the colon.
The tumour in the lung can no longer be measured because it's now too small and one in the liver is under 2cm while the other is 3cm.
'So far I've had a very positive response to treatment - better than my doctor thought I would have,' she said. 'It's really been a miracle and I'm so glad it's been working so well.'
Up until a few weeks ago, Samantha thought she was already nine months into those two to three years, but the doctor reassured her it 'doesn't quite work like that'.
She explained after every check-up from the scans the clock restarts. The time doesn't start from the diagnosis, it restarts from the latest scan.
This news was a sigh of relief for Samantha who feels like she's been given extra time.
However, there is still the looming possibility that this could change at any moment. Luckily Samantha is on her first line of treatment options.
When she was diagnosed the doctor said if treatment doesn't work she'll likely only have 12 months to live. But if it does work, she will have likely two to three years to live. This time resets with every checkup if the treatment continues to work
At this stage, she'll require treatment for the rest of her life because at this stage if doctors stopped treatment the tumours would grow back.
'My doctor said to me if treatment doesn't work, you're looking at less than 12 months. If it does work, I hope to buy you two to three years', which is obviously not what anyone wants to hear,' she said.
'My mum died of breast cancer when I was 10. It started at stage one or two then elevated to stage four. It was very aggressive and moved into her liver, then she really went downhill quick.
'So I associate cancer in the liver with really bad news because I saw it first hand.'
In terms of what caused the cancer, unfortunately it was random and a case of bad luck. There's nothing Samantha could've done different to prevent the tumours from growing.
'I have surprised myself with the fact that I had [the ability to do this] and push through. I've been able to come to terms and accept that I have cancer,' she continued.
'If you had told me last year that I'll be diagnosed with cancer and that I'm actually going to be fine emotionally, I wouldn't have believed you. You'll be surprised what you can do.'
Luckily throughout treatment she's experienced minimal side effects besides fatigue.
But the immunotherapy treatment left her with an acne-like rash covering her whole body, including her scalp and tongue.
'The doctor said my rash was the worst one they've seen, but it's a sign that the treatment is working. So I found comfort in that,' she said.
In terms of what caused the cancer, unfortunately it was random and was a case of bad luck. There's nothing Samantha could've done different to prevent the tumours from growing
WHAT ARE THE SYMPTOMS OF COLORECTAL CANCER?Colorectal cancer is a type of cancer that affects the colon (large intestine) or rectum. It is one of the most common types of cancer worldwide.
Colorectal cancer often has no symptoms in the early stages. Regular screenings are important to catch the disease early and begin treatment.
Common symptoms include:
Source: WHO
AdvertisementDespite the awful diagnosis and prognosis Samantha's received, she feels 'fitter, stronger and better' than ever before.
'One of the girls at work brought it to my attention. She told me, "You have so much more life and vibrancy in you, you seem so much stronger compared to when I first met you when all this started happening",' Samantha recalled.
She also feels confident because she has her youth on her side to combat against the deadly cancer and bounce back from treatment quickly.
To keep herself fit and healthy, she goes for 5km walks every day and eats fresh, clean food.
'I don't look like a cancer patient either - you wouldn't know I'm sick by looking at me,' she said, adding: 'I've tried to keep life as normal as possible too.
'I heard the phrase, "Everyone's terminal, I just have it in writing" and it really changed my mindset. This is it, this is the life you've got and it can change for anyone at any time like it did for me.
'Right now, besides the cancer, I'm healthy enough to be able to do things and I maximise on this like you have no idea.
'I spend as much time as possible with the people that I love doing the things the I love because I know that's what matters most.
'I don't want to get to a point when I'm so ill that I'm bedridden and then start to think "why didn't I do things I enjoy earlier?" I want to make sure I live as fully as possible.'
Samantha also urges everyone to advocate for their health and to be in touch with your body to be able to notice any changes.
'If something feels off or if you're not sure, visit a doctor,' she said.
READ MORE: Young nurse's warning to Aussies about why everyone must have a bedframe to prevent dangerous mould
Young woman, 30, diagnosed with terminal cancer after feeling 'bloated and tired' reveals how she will spend her final days
Everything You Need To Know About Pancreatic Cancer
Pancreatic cancer affects the pancreas, a crucial organ located behind the stomach. The organ's location can make this cancer harder to detect, leading to diagnosis in advanced stages.
According to the American Cancer Society, pancreatic cancer makes up about 3 percent of cancer diagnoses in the United States and 7 percent of cancer deaths.
Read on to learn about pancreatic cancer, its symptoms, causes, and treatment.
The pancreas plays an essential role in digestion by producing enzymes that the body needs to digest fats, carbohydrates, and proteins.
The pancreas also produces two important hormones: glucagon and insulin. These hormones are responsible for controlling glucose (sugar) metabolism. Insulin helps cells metabolize glucose to make energy, and glucagon helps raise glucose levels when they are too low.
There are two main types of pancreatic cancer, based on the kind of cell they start in:
Pancreatic cancer often doesn't cause symptoms until it reaches advanced stages. As a result, there typically aren't any early signs of pancreatic cancer.
Even at more advanced stages, some of the most common pancreatic cancer symptoms can be subtle.
As it progresses, pancreatic cancer can cause the following symptoms:
Pancreatic cancer can also affect your blood sugar. In some cases, this might lead to diabetes (or the worsening of preexisting diabetes).
Keep in mind that the above symptoms can be caused by a range of less-serious health concerns.
Learn more about the signs and symptoms of pancreatic cancer.
The cause of pancreatic cancer is unknown.
Pancreatic cancer occurs when abnormal cells begin to grow within the pancreas and form tumors, but it's unclear why this happens.
Typically, healthy cells grow and die in moderate numbers. In the case of cancer, there's an increase in the production of abnormal cells. These cells eventually take over healthy cells.
While the underlying cause of pancreatic cancer is unknown, certain factors may increase your risk of developing it.
These include:
Certain genetic variations and mutations can cause conditions that may also increase your risk of pancreatic cancer. Some of these conditions include:
Learn more about the hereditary factors that affect pancreatic cancer risk.
Early diagnosis significantly increases the chances of recovery. That's why it's best to see a healthcare professional as soon as possible if you notice any unusual symptoms, especially if you have any risk factors for pancreatic cancer.
To make a diagnosis, your care team will review your symptoms and medical history. They may order one or more tests to check for pancreatic cancer, such as:
When pancreatic cancer is discovered, doctors will likely perform additional tests to determine whether the cancer has spread. These might include imaging tests, such as a PET scan, or blood tests.
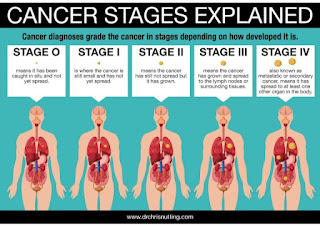
They'll use the results of these tests to establish the stage of the cancer. Staging helps explain how advanced the cancer is, which will help determine the best treatment option.
The stages of pancreatic cancer are:
Here's a closer look at the different stages of pancreatic cancer.
Pancreatic cancer stage 4Stage 4 pancreatic cancer has spread beyond the original site to distant sites, like other organs, the brain, or bones.
Pancreatic cancer is often diagnosed at this late stage because it rarely causes symptoms until it has spread to other sites.
Symptoms you might experience at this stage include:
Stage 4 pancreatic cancer can't be cured, but treatments can relieve symptoms and prevent complications from the cancer.
Pancreatic cancer stage 3Stage 3 pancreatic cancer is a tumor in the pancreas and possibly nearby sites, such as lymph nodes or blood vessels.
Symptoms of stage 3 pancreatic cancer may include:
Stage 3 pancreatic cancer is difficult to cure, but treatments can help prevent the spread of the cancer and ease symptoms. These treatments may include:
The majority of people with this stage of the cancer will have a recurrence. That's likely due to the fact that micrometastases, or small areas of undetectable cancer growth, have spread beyond the pancreas as the time of detection and aren't removed during surgery.
Pancreatic cancer stage 2Stage 2 pancreatic cancer is cancer that remains in the pancreas but may have spread to a few nearby lymph nodes or blood vessels.
This stage is divided into two subcategories, depending on where the cancer is and the size of the tumor:
Symptoms of stage 2 pancreatic cancer tend to be very subtle and may include:
Treatment may include:
Your doctor may use a combination of these approaches to help shrink the tumor and prevent possible metastases.
Pancreatic cancer stage 1Stage 1 pancreatic cancer involves a tumor that's only in the pancreas. This stage is divided into two subcategories, depending on the size of the tumor:
Stage 1 pancreatic cancer typically doesn't cause any noticeable symptoms.
If detected at this stage, pancreatic cancer may be curable with surgery.
Pancreatic cancer stage 0This is the earliest stage of pancreatic cancer, though it may not necessarily involve cancer. It just means that abnormal cells have been detected, and they could potentially become cancerous in the future. This stage doesn't involve any symptoms.
Read more about pancreatic cancer staging.
Treating pancreatic cancer involves two main goals: to kill cancerous cells and prevent the cancer from spreading. The most appropriate treatment option will depend on the stage of the cancer.
The main treatment options include:
In some cases, a doctor might recommend combining multiple treatment options. For example, chemotherapy might be done before surgery.
For advanced-stage pancreatic cancer, treatment options might focus more on pain relief and keeping symptoms as manageable as possible.
Pancreatic cancer surgeryTumors confined to the "head and neck" of the pancreas can be removed with a procedure called the Whipple procedure (pancreaticoduodenectomy).
In this procedure, the first part, or the "head" of the pancreas and about 20 percent of the "body," or the second part, are removed. The bottom half of the bile duct and the first part of the intestine are also removed.
In a modified version of this surgery, a part of the stomach is also removed.
A survival rate is a percentage of how many people with the same type and stage of a cancer are still alive after a specific amount of time. This number doesn't indicate how long people may live. Instead, it helps gauge how successful treatment for a cancer might be.
Many survival rates are given as a 5-year percentage, which refers to the percentage of people alive 5 years after being diagnosed or starting treatment.
It's important to keep in mind that survival rates aren't definitive and can vary greatly from person to person depending on age, overall health, and how the cancer progresses. As a result, they also can't determine an individual's life expectancy.
Survival rates for pancreatic cancer are typically provided for localized, regional, and distant stages:
Here's a look at the 1-, 5-, and 10-year relative survival rates from diagnosis for each stage.
If you or a loved one was recently diagnosed with pancreatic cancer, it's understandable to immediately wonder about life expectancy, but this depends on a range of factors that vary greatly from person to person. Your healthcare team can provide the most accurate estimate based on these factors.
Read more about life expectancy and pancreatic cancer.
Pancreatic cancer prognosisIt's worth noting that survival rates are based on people who were first treated at least 5 years ago. Someone being diagnosed today may have a better survival rate thanks to advances in cancer treatments.
That said, pancreatic cancer is still considered difficult to treat, largely because it often isn't found until it's spread to other parts of the body.
It's still not clear what causes pancreatic cancer, so there's no reliable way to prevent it.
While certain things might increase your risk of developing pancreatic cancer, some of these — like your family history and age — can't be changed.
But a few lifestyle changes may help reduce your risk:
If you're experiencing symptoms you think might indicate pancreatic cancer, talk with a healthcare professional as soon as possible, especially if you have an increased risk of pancreatic cancer. While many conditions can have similar symptoms, pancreatic cancer responds best to treatment when caught in its earlier stages.




Comments
Post a Comment