Metastatic breast cancer in the lungs: Symptoms, outlook, and more
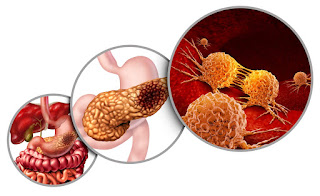
Everything You Need To Know About Pancreatic Cancer
Pancreatic cancer affects the pancreas, a crucial organ located behind the stomach. The organ's location can make this cancer harder to detect, leading to diagnosis in advanced stages.
According to the American Cancer Society, pancreatic cancer makes up about 3 percent of cancer diagnoses in the United States and 7 percent of cancer deaths.
Read on to learn about pancreatic cancer, its symptoms, causes, and treatment.
The pancreas plays an essential role in digestion by producing enzymes that the body needs to digest fats, carbohydrates, and proteins.
The pancreas also produces two important hormones: glucagon and insulin. These hormones are responsible for controlling glucose (sugar) metabolism. Insulin helps cells metabolize glucose to make energy, and glucagon helps raise glucose levels when they are too low.
There are two main types of pancreatic cancer, based on the kind of cell they start in:
Pancreatic cancer often doesn't cause symptoms until it reaches advanced stages. As a result, there typically aren't any early signs of pancreatic cancer.
Even at more advanced stages, some of the most common pancreatic cancer symptoms can be subtle.
As it progresses, pancreatic cancer can cause the following symptoms:
Pancreatic cancer can also affect your blood sugar. In some cases, this might lead to diabetes (or the worsening of preexisting diabetes).
Keep in mind that the above symptoms can be caused by a range of less-serious health concerns.
Learn more about the signs and symptoms of pancreatic cancer.
The cause of pancreatic cancer is unknown.
Pancreatic cancer occurs when abnormal cells begin to grow within the pancreas and form tumors, but it's unclear why this happens.
Typically, healthy cells grow and die in moderate numbers. In the case of cancer, there's an increase in the production of abnormal cells. These cells eventually take over healthy cells.
While the underlying cause of pancreatic cancer is unknown, certain factors may increase your risk of developing it.
These include:
Certain genetic variations and mutations can cause conditions that may also increase your risk of pancreatic cancer. Some of these conditions include:
Learn more about the hereditary factors that affect pancreatic cancer risk.
Early diagnosis significantly increases the chances of recovery. That's why it's best to see a healthcare professional as soon as possible if you notice any unusual symptoms, especially if you have any risk factors for pancreatic cancer.
To make a diagnosis, your care team will review your symptoms and medical history. They may order one or more tests to check for pancreatic cancer, such as:
When pancreatic cancer is discovered, doctors will likely perform additional tests to determine whether the cancer has spread. These might include imaging tests, such as a PET scan, or blood tests.
They'll use the results of these tests to establish the stage of the cancer. Staging helps explain how advanced the cancer is, which will help determine the best treatment option.
The stages of pancreatic cancer are:
Here's a closer look at the different stages of pancreatic cancer.
Pancreatic cancer stage 4Stage 4 pancreatic cancer has spread beyond the original site to distant sites, like other organs, the brain, or bones.
Pancreatic cancer is often diagnosed at this late stage because it rarely causes symptoms until it has spread to other sites.
Symptoms you might experience at this stage include:
Stage 4 pancreatic cancer can't be cured, but treatments can relieve symptoms and prevent complications from the cancer.
Pancreatic cancer stage 3Stage 3 pancreatic cancer is a tumor in the pancreas and possibly nearby sites, such as lymph nodes or blood vessels.
Symptoms of stage 3 pancreatic cancer may include:
Stage 3 pancreatic cancer is difficult to cure, but treatments can help prevent the spread of the cancer and ease symptoms. These treatments may include:
The majority of people with this stage of the cancer will have a recurrence. That's likely due to the fact that micrometastases, or small areas of undetectable cancer growth, have spread beyond the pancreas as the time of detection and aren't removed during surgery.
Pancreatic cancer stage 2Stage 2 pancreatic cancer is cancer that remains in the pancreas but may have spread to a few nearby lymph nodes or blood vessels.
This stage is divided into two subcategories, depending on where the cancer is and the size of the tumor:
Symptoms of stage 2 pancreatic cancer tend to be very subtle and may include:
Treatment may include:
Your doctor may use a combination of these approaches to help shrink the tumor and prevent possible metastases.
Pancreatic cancer stage 1Stage 1 pancreatic cancer involves a tumor that's only in the pancreas. This stage is divided into two subcategories, depending on the size of the tumor:
Stage 1 pancreatic cancer typically doesn't cause any noticeable symptoms.
If detected at this stage, pancreatic cancer may be curable with surgery.
Pancreatic cancer stage 0This is the earliest stage of pancreatic cancer, though it may not necessarily involve cancer. It just means that abnormal cells have been detected, and they could potentially become cancerous in the future. This stage doesn't involve any symptoms.
Read more about pancreatic cancer staging.
Treating pancreatic cancer involves two main goals: to kill cancerous cells and prevent the cancer from spreading. The most appropriate treatment option will depend on the stage of the cancer.
The main treatment options include:
In some cases, a doctor might recommend combining multiple treatment options. For example, chemotherapy might be done before surgery.
For advanced-stage pancreatic cancer, treatment options might focus more on pain relief and keeping symptoms as manageable as possible.
Pancreatic cancer surgeryTumors confined to the "head and neck" of the pancreas can be removed with a procedure called the Whipple procedure (pancreaticoduodenectomy).
In this procedure, the first part, or the "head" of the pancreas and about 20 percent of the "body," or the second part, are removed. The bottom half of the bile duct and the first part of the intestine are also removed.
In a modified version of this surgery, a part of the stomach is also removed.
A survival rate is a percentage of how many people with the same type and stage of a cancer are still alive after a specific amount of time. This number doesn't indicate how long people may live. Instead, it helps gauge how successful treatment for a cancer might be.
Many survival rates are given as a 5-year percentage, which refers to the percentage of people alive 5 years after being diagnosed or starting treatment.
It's important to keep in mind that survival rates aren't definitive and can vary greatly from person to person depending on age, overall health, and how the cancer progresses. As a result, they also can't determine an individual's life expectancy.
Survival rates for pancreatic cancer are typically provided for localized, regional, and distant stages:
Here's a look at the 1-, 5-, and 10-year relative survival rates from diagnosis for each stage.
If you or a loved one was recently diagnosed with pancreatic cancer, it's understandable to immediately wonder about life expectancy, but this depends on a range of factors that vary greatly from person to person. Your healthcare team can provide the most accurate estimate based on these factors.
Read more about life expectancy and pancreatic cancer.
Pancreatic cancer prognosisIt's worth noting that survival rates are based on people who were first treated at least 5 years ago. Someone being diagnosed today may have a better survival rate thanks to advances in cancer treatments.
That said, pancreatic cancer is still considered difficult to treat, largely because it often isn't found until it's spread to other parts of the body.
It's still not clear what causes pancreatic cancer, so there's no reliable way to prevent it.
While certain things might increase your risk of developing pancreatic cancer, some of these — like your family history and age — can't be changed.
But a few lifestyle changes may help reduce your risk:
If you're experiencing symptoms you think might indicate pancreatic cancer, talk with a healthcare professional as soon as possible, especially if you have an increased risk of pancreatic cancer. While many conditions can have similar symptoms, pancreatic cancer responds best to treatment when caught in its earlier stages.
Whipple Procedure: Will It Cure Pancreatic Cancer?
A Whipple procedure is the main surgery used to treat tumors in the head of the pancreas. Also called a pancreaticoduodenectomy, it's named after Allen Whipple, MD, a Columbia University surgeon. In 1935, he became the first American to perform the operation.
Among common cancers, pancreatic cancer has one of the poorest prognoses. Because pancreatic cancer often grows and spreads long before it causes any symptoms, only about 6% of people who are diagnosed live 5 years after diagnosis.
If you have cancer in your pancreas or nearby organs, the Whipple procedure may be the only way to extend your life and potentially cure you. Those who undergo a successful Whipple procedure may boost their 5-year survival rate up to 25%.
The Whipple procedure involves removing the head (wide part) of the pancreas, which is connected to the top part of the small intestine (duodenum). Your doctor may also take out the:
Surgeons reconnect the small intestine, bile duct, and pancreas after they remove tumors or other damaged tissue.
The Whipple procedure involves removal of the head of the pancreas, which is connected to the top part of the small intestine. Surgeons reconnect the small intestine, bile duct, and pancreas after they remove tumors or other damaged tissue. (Photo credit: iStock/Getty Images)
About 20% of people withpancreatic cancer are eligible for the Whipple procedure and other surgeries. These are usually people whose tumors are confined to the head of the pancreas and haven't spread to nearby major blood vessels, or the liver,lungs, or abdominal cavity. Intensive testing is usually necessary to identify possible candidates for the Whipple procedure.
Most people who get this operation have pancreatic cancer. But the Whipple procedure is sometimes used to treat health conditions such as:
The Whipple procedure isn't an option for the 40% of newly diagnosed people whose tumors have spread (metastasized) beyond the pancreas. Only rarely is it an option for the 40% of patients with locally advanced disease that has spread to adjacent areas such as the superior mesenteric vein and artery, or for those whose tumors have spread to the body or tail of the pancreas.
You'll meet with your surgeon ahead of time to go over the next steps. This is a good time to bring up any concerns or ask about how the procedure may affect your life.
If you have cancer, you may need treatment with radiation or chemotherapy before your operation. When you get a date for your Whipple procedure, you'll need to stop taking certain medications and herbal supplements. Your doctor will let you know which ones.
The day before you go to the hospital, you may need to:
Once you get to the hospital, a nurse will put a needle and tube into a vein in your arm. You may hear this called an intravenous (IV) line. The IV makes it easier for your health care team to put fluids and medication into your arm before or during surgery. Your doctor may put a numbing drug in your spine. Also called an epidural catheter, this spinal shot can lessen post-surgery pain.
There are a few different ways to do the Whipple procedure. The types of surgery offered include:
Compared to an open surgery, a laparoscopic or minimally invasive procedure may result in less blood loss, a shorter hospital stay, a quicker recovery, and fewer complications.
You'll get general anesthesia during surgery. This is a type of medication that puts you to sleep. When you're no longer awake, someone on your surgical team will put a tube into your bladder. This is called a urinary catheter, and it's used to drain your pee during the procedure.
Your surgery may take 4-12 hours, but it depends on what your surgical team needs to do. They may not know how complex your case is until they take a look during the procedure.
Steps of a Whipple procedure:
After surgery, you may need to stay in the hospital for a week or so before returning home. Your doctor will give you prescription or over-the-counter painkillers for any discomfort you may have during recovery. They'll let you know how often to use these medications.
Right after the procedure, you'll wake up in a special recovery room. A nurse will check on you before they move you to a general area. During your hospital stay, someone on your health care team will watch for signs of infections or other problems.
Most people can recover at home. But older adults or people with other health issues may need to go to a special rehabilitation facility to get better.
At first, you may only be able to eat small amounts of easily digestible food. You may need to take pancreatic enzymes -- medication that helps you break down food -- on a short-term or long-term basis to assist with digestion. Diarrhea is a common problem during the 2 or 3 months it usually takes for the rearranged digestive tract to fully recover.
You should be able to go back to doing normal activities around 4-6 weeks after surgery. But how long it takes you to recover depends on your overall health and the kind of surgery you have.
Around 1 in 3 people who get this surgery have a complication afterward. Some are mild, while others are more serious. One of the most common things to happen right after the Whipple procedure is the development of false channels (fistulas) and leakage from the site of the bowel reconnection. Infections, bleeding, and slow stomach emptying after meals can also happen after the procedure.
Other possible surgical complications include:
Overall, about 20%-25% of people who get the Whipple procedure are alive 5 years after surgery. But even if your surgeon removes the visible tumor, it's possible for cancer cells to spread elsewhere in the body. This can be fatal down the road even if your surgery is successful.
In the past few decades, there have been a lot of improvements in diagnosis, staging, surgical techniques, anesthesia, and postoperative care for the Whipple procedure. As a result, the short-term death rate has dropped to less than 4% in people who get surgery at cancer centers by experienced surgeons. At some major centers, the reported death rate is less than 1%. But it may still be more than 15% for people who get treatment at a small hospital or by less experienced surgeons.
The 5-year survival rate is higher if you have node-negative cancer (when cancer hasn't spread to nearby lymph nodes) than for people who have node-positive cancer.
Regardless of node status, most people with pancreatic cancer receive chemotherapy, radiation, or both before or after surgery. But cancer specialists have differing opinions on the best combination and the best drugs to use. Recent trials have shown improved outcomes with chemotherapy before surgery and with different chemotherapy regimens before and after surgery.
The Whipple procedure may help people with pancreatic cancer or other cancers live longer; however, it's a difficult surgery that may come with complications. An experienced surgeon can go over the pros and cons with you and let you know how the operation may change your daily life.
What is the life expectancy of a Whipple surgery?
If you don't have pancreatic cancer, you may have a normal life expectancy after surgery. People diagnosed with common kinds of advanced pancreatic cancer may live around 2 years afterward. But how long you'll live depends on why you get the procedure in the first place and how far your cancer has spread.
Can you live a normal life after the Whipple procedure?
You can usually go back to your regular daily activities around 4-6 weeks after surgery. But you may need to take pancreatic enzymes to aid in digestion or make long-term diet changes.
How serious is the Whipple procedure?
This is a very complex operation that should be done by a skilled surgeon. Doctors with experience in the Whipple procedure typically work at big cancer centers.
Why would someone need a Whipple procedure?
Most people who need this surgery get it to remove tumors related to pancreatic cancer. But this operation is sometimes used to treat pancreatic inflammation or cysts along with cancers of the bile duct, small intestine, or nearby organs.
Six Signs In Your Poo That Could Be Red Flags For Pancreatic Cancer
This article contains affiliate links, we will receive a commission on any sales we generate from it. Learn more This Morning: Dr Zoe explains symptoms of pancreatic cancerPancreatic cancer is the 10th most common cancer in the UK. As with all cancers, spotting symptoms as early as possible could save your life.
It doesn't usually cause any symptoms in the early stages, but as the cancer grows, symptoms can start. Jaundice, loss of appetite, feeling tired and a high temperature are just some of the symptoms of pancreatic cancer listed by the NHS.
But a change in the way you poo is also worth noting. Symptoms in your poo to spot include:
Pancreatic Cancer Action explains: "People with pancreatic cancer sometimes experience constipation (when your stools are very firm and difficult to push out, sometimes accompanied by stomach pain) or diarrhoea (passing of watery stools more than three times a day).
"Stools can also be large, pale, smelly and float. This is because there is too much fat in the stool as food is not digested properly."
Constipation and diarrhoea are quite common, but if a change in your bowels keeps happening or lasts longer than a week, you should see your GP.
The charity adds: "It does not mean you have pancreatic cancer and your GP may be able to resolve your symptoms easily."
The common symptoms of pancreatic cancer, according to Cancer Research UK, are:
People describe the pain as a dull pain that feels like it's boring into you. It can begin in the tummy area and spread around to the back.
It can also be worse when you lie down and is better if you sit forward. It can also be worse after meals.
Jaundice is yellowing of the skin and whites of the eyes, but it can also cause your wee to be darker than normal and make your stools lighter in colour.
Losing a lot of weight for no apparent reason should be cause for concern.
Other signs to be aware of are:
But it's important to understand the symptoms of pancreatic cancer can be caused by many different conditions, including irritable bowel syndrome or indigestion.






Comments
Post a Comment