12 Types of Common Cancers in Men (With Screening)
What Is Lymphoma?
Lymphoma is cancer that begins in infection-fighting cells of the immune system, called lymphocytes. These cells are in the lymph nodes, spleen, thymus, bone marrow, and other parts of the body. When you have lymphoma, lymphocytes change and grow out of control.
There are two main types of lymphoma:
Non-Hodgkin and Hodgkin lymphoma involve different types of lymphocyte cells. Every type of lymphoma grows at a different rate and responds differently to treatment.
Lymphoma is very treatable, and the outlook can vary depending on the type of lymphoma and its stage. Your doctor can help you find the right treatment for your type and stage of the illness.
Lymphoma is different from leukemia. Each of these cancers starts in a different type of cell.
Lymphoma is also not the same as lymphedema, which is a collection of fluid that forms in body tissues when there is damage or blockage to the lymph system.
Scientists don't know what causes lymphoma in most cases.
You might be more at risk if you:
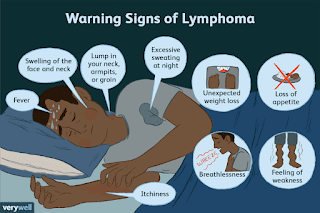
Warning signs of lymphoma include:
Many of these symptoms can also be warning signs of other illnesses. See your doctor to find out for sure if you have lymphoma.
Before you have any tests, your doctor will want to know:
Your doctor will do a physical exam, including a check for swollen lymph nodes. This symptom doesn't mean you have cancer. Most of the time, an infection -- unrelated to cancer -- causes swollen lymph nodes.
You might get a lymph node biopsy to check for cancer cells. For this test, a doctor will remove all or part of a lymph node, or use a needle to take a small amount of tissue from the affected node.
You might also have one of these tests to help diagnose, stage, or manage lymphoma:
The treatment you get depends on what type of lymphoma you have and its stage.
The main treatments for non-Hodgkin lymphoma are:
The main treatments for Hodgkin lymphoma are:
If these treatments don't work, you might have a stem cell transplant. First you'll get very high doses of chemotherapy. This treatment kills cancer cells, but it also destroys stem cells in your bone marrow that make new blood cells. After chemotherapy, you will get a transplant of stem cells to replace the ones that were destroyed.
Two types of stem cell transplants can be done:
Lymphoma treatment can cause side effects. Talk to your medical team about ways to relieve any symptoms you have.
Also ask your doctor about changes to your diet and exercise that can help you feel better during your treatment. Ask a dietitian for help if you're not sure what types of food to eat. Exercises like walking or swimming can relieve fatigue and help you feel better during treatments like chemotherapy and radiation. You might also try alternative therapies like relaxation, biofeedback, or guided imagery to help relieve pain.
Treatments have improved a lot, and many people do very well after treatment. Your doctor will talk to you about a survivorship care plan. Your outlook depends on:
You can get support from people who have gone through this kind of illness.
Contact the Leukemia & Lymphoma Society or Lymphoma Research Foundation to learn more.
What To Know About Mantle Cell Lymphoma (MCL)
Mantle cell lymphoma is a rare and aggressive type of non-Hodgkin's lymphoma.
Lymphoma is a type of cancer that starts in your white blood cells. Mantle cell lymphoma (MCL) is a rare lymphoma.
Read on to learn about the causes and symptoms of MCL and how doctors diagnose and treat this type of cancer.
There are two forms of lymphoma: Hodgkin's and non-Hodgkin's. MCL is a type of non-Hodgkin's lymphoma.
More than 80,600 people are diagnosed with non-Hodgkin's lymphoma each year in the United States. Only about 5% of non-Hodgkin's lymphomas are MCL.
While some forms of MCL are slow-growing, MCL is usually aggressive, and doctors often don't diagnose it until it has spread throughout the body. It may cause symptoms based on the location of the spread, such as intestinal blockage if the tumor spreads to the digestive tract.
Causes and risk factorsMCL results from a genetic mutation, but the cause is usually unknown. A family history may increase your risk of developing it.
It occurs more often in males and adults ages 60–70 years.
You may experience certain symptoms depending on where the cancer has spread. Blood cancers can also cause systemic symptoms, like feeling generally unwell.
Signs and symptoms of MCL may include:
Some people with mantle cell lymphoma won't have any obvious symptoms until their disease has spread throughout their body.
Doctors diagnose MCL based on the results of a biopsy, such as a lymph node biopsy.
A doctor typically diagnoses MCL by performing the following tests and procedures:
Doctors stage MCL like they do other types of non-Hodgkin's lymphoma.
However, non-Hodgkin's lymphoma does not necessarily start at stage 1 and progress to each of the other stages. The stage indicates the location of the disease.
Treatment will depend on the severity of your condition and how aggressive your lymphoma is.
If your cancer is indolent (slow growing), a doctor might suggest monitoring the cancer (watchful waiting) instead of undergoing immediate treatment. However, most people with MCL have aggressive cancers that require immediate treatment.
Treatment usually involves a combination of medications. This can include:
Some people may experience side effects from MCL treatment. Side effects can include:
If you have side effects from treatment, it's best to discuss them with your healthcare team. They may be able to help you manage or prevent them.
MCL is an aggressive form of cancer that's difficult to treat. By the time doctors diagnose the cancer, it has often spread to other areas of the body. There is no curative treatment for all people with MCL, though some people may experience complete remission with an allogeneic stem cell transplant.
The median life expectancy is 1.8 to 9.4 years from diagnosis, depending on how quickly it progresses.
It's important to remember that each person is different, and the survival rates are based on averages of people diagnosed with MCL. As researchers discover newer treatments, the outlook for those with this type of lymphoma is likely to improve.
ComplicationsPeople with MCL are likely to develop complications from their disease. Some of these include:
Recovery from MCL can depend on individual factors and how advanced your disease is.
Most people go into remission after the initial treatment of chemotherapy with or without a stem cell transplant. However, the cancer usually comes back. If this happens, you can develop treatment resistance, which means the therapies that worked before might not be as effective.
What is the survival rate of mantle cell lymphoma?According to a 2024 study that divided participants into under and over age 65 years, researchers found that 82% of people with MCL under 65 years were alive 5 years later, compared with 55% of those older than 65 years.
How curable is mantle cell lymphoma?There is currently no cure for all people with MCL. But treatment can lead to a longer-term remission (reduction or disappearance of disease activity) in some people. Some people may experience complete remission with an allogeneic stem cell transplant.
Is mantle cell lymphoma an aggressive cancer?MCL is usually aggressive and requires immediate treatment.
What are the signs of mantle cell lymphoma?Some people may not have signs of MCL until the cancer has spread throughout the body. You may have symptoms that include fatigue, night sweats, and swollen lymph nodes. You may have additional symptoms depending on where the cancer has spread.
MCL is a type of non-Hodgkin's lymphoma that is typically aggressive. It may not cause symptoms until it has spread throughout the body. Diagnosis requires various blood and imaging tests.
Treatment typically includes a combination of medications, such as chemotherapy and targeted therapies.
Computer Model Can Find Signs Of Lymph Node Cancer In 90% Of Cases
Medical image analysis using AI has developed rapidly in recent years. Now, one of the largest studies to date has been carried out using AI-assisted image analysis of lymphoma, cancer of the lymphatic system. Researchers at Chalmers University of Technology in Sweden, have developed a computer model that can successfully find signs of lymph node cancer in 90 percent of cases.
New computer-aided methods for interpreting medical images are being developed for various medical conditions. They can reduce the workload for radiologists, by giving a second opinion or ranking which patients need treatment the fastest.
An AI-based computer system for interpreting medical images also contributes to increased equality in healthcare by giving patients access to the same expertise and being able to have their images reviewed within a reasonable time, regardless of which hospital they are in. Since an AI system has access to much more information, it also makes it easier in rare diseases where radiologists rarely see images."
Ida Häggström, Associate Professor, Department of Electrical Engineering, Chalmers University
In close collaboration with Sahlgrenska Academy at the University of Gothenburg and Sahlgrenska University Hospital, she has participated in the development of medical imaging in the field of cancer, as well as in a number of other medical conditions, such as cardiovascular disease, stroke and osteoporosis.
Large study to track cancer in the lymphatic systemTogether with clinically active researchers at, among others, Memorial Sloan Kettering Cancer Center in New York, Ida Häggström has developed a computer model that was recently presented in The Lancet Digital Health.
"Based on more than 17,000 images from more than 5,000 lymphoma patients, we have created a learning system in which computers have been trained to find visual signs of cancer in the lymphatic system," says Häggström.
In the study, the researchers examined image archives that stretched back more than ten years. They compared the patients' final diagnosis with scans from positron emission tomography (PET) and computed tomography (CT) taken before and after treatment. This information was then used to help train the AI computer model to detect signs of lymph node cancer in an image.
Supervised trainingThe computer model that Ida Häggström has developed is called Lars, Lymphoma Artificial Reader System, and is a so-called deep learning system based on artificial intelligence. It works by inputting an image from positron emission tomography (PET) and analysing this image using the AI model. It is trained to find patterns and features in the image, in order to make the best possible prediction of whether the image is positive or negative, i.E. Whether it contains lymphoma or not.
"I have used what is known as supervised training, where images are shown to the computer model, which then assesses whether the patient has lymphoma or not. The model also gets to see the true diagnosis, so if the assessment is wrong, the computer model is adjusted so that it gradually gets better and better at determining the diagnosis," says Häggström.
In practice, what does it actually mean that the computer model uses artificial intelligence and deep learning to make a diagnosis?
"It's about the fact that we haven't programmed predetermined instructions in the model about what information in the image it should look at, but let it teach itself which image patterns are important in order to get the best predictions possible.
Support for radiologistsIda Häggström describes the process of teaching the computer to detect, in this case, cancer in the images as time-consuming, and says that it has taken several years to complete the study. One challenge has been to produce such a large amount of image material. It has also been challenging to adapt the computer model so that it can distinguish between cancer and the temporary treatment-specific changes that can be seen in the images after radiotherapy and chemotherapy.
"In the study, we estimated the accuracy of the computer model to be about ninety per cent, and especially in the case of images that are difficult to interpret, it could support radiologists in their assessments."
However, there is still a great deal of work to be done to validate the computer model if it is to be used in clinical practice.
"We have made the computer code available now so that other researchers can continue to work on the basis of our computer model, but the clinical tests that need to be done are extensive," says Häggström.
Source:
Journal reference:
Häggström, I., et al. (2023). Deep learning for [18F]fluorodeoxyglucose-PET-CT classification in patients with lymphoma: a dual-centre retrospective analysis. The Lancet Digital Health. Doi.Org/10.1016/s2589-7500(23)00203-0.

Comments
Post a Comment