What Is Cancer? Symptoms, Signs, Types & Causes
Lung Disease
Increasing level of pollution has made breathing in urban areas very difficult, raising the incidence of respiratory problems. Out of the world's top 20 cities with polluted air, 13 belong to India and according to the World health Organisation (WHO) report published in 2011, lung diseases rank 2ndin the list of top 20 causes of death. Naturally, lung disease is a big health issue that needs to be addressed. Here are some facts about lung disease you should know about.To understand the condition of your lungs, you need to first understand how the lungs function. Lungs are soft organs present on both right and left side of the chest. They are protected by a had covering called the ribcage. Each lung is made of sections called lobes. The main function of the lungs is to make oxygen available for purifying blood and to and eliminate carbondioxide from impure blood or deoxygenated blood. So when you breathe, air travels down your windpipe (trachea). The windpipe bifurcates with each branch entering each of the lungs. Into the lungs, the windpipe is further branched to tubes called bronchioles that end in small sacs called alveoli, where the inhaled air reaches for delivering oxygen.
A lung disease or disorder occurs in the various structures of lungs and disrupts its functioning. It can vary from a mild common cold to life-threatening conditions like pneumonia and cancer. Lung disease can be caused by infections, inflammation, obstruction of airways, decreased lung function, problems related to pulmonary circulation, etc. Smoking, infections, air pollution, genetics, exposure to asbestos, etc. Can cause various lung diseases.
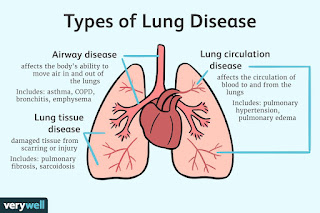
TypesThe common as well as rare types of lung disease include -
Causes'In any form of lung disease mainly the breathing gets affected,' says Dr Animesh Arya, Senior Consultant, Respiratory Medicine, Delhi based Sri Balaji Action Medical Institute. Here are some common forms of lung diseases he explains. 1. Asthma:It is the most common lung disease triggered by allergies, infections and pollutants that harm the airways and cause inflammation. 2. Acute bronchitis: Bronchitis is the inflammation of the air passage. Acute bronchitis is caused by viral or bacterial respiratory infections. 3. Chronic Obstructive Pulmonary Disease (COPD): It a group of diseases that causes breathing difficulties and interfere with the exhalation process of breathing. 4. Chronic bronchitis: It is a type of COPD caused mainly due to smoking. 5. Emphysema: It is a COPD caused by environmental factors and may also be triggered by allergens or organisms that cause diseases like pneumonia and tuberculosis. Apart from these common forms of lung diseases, other rare lung diseases include: 6. Cystic fibrosis: It is rare lung disease caused by genetic mutation that results in excess mucus production causing blockage of airways. 7. Acute respiratory distress syndrome (ARDS): It is a medical emergency caused as a result of lung injury due to a severe illness. 8. Lung cancer: It can affect any part of the lung. It is mainly caused due to smoking. Here are 10 common symptoms of lung cancer you need to know. 9. Interstitial lung disease: This is a group of diseases affecting the interstitium, a thin lining separating the air sacs.
Symptoms'Bronchitis, asthma, COPD, lung infections and pulmonary fibrosis have similar symptoms even though they are very different in nature,' says Dr Arya. He lists a few common symptoms of lung diseases:
In most cases, chronic cough, chest pain and breathing difficulties necessitate a lung function test. But your doctor might first take a look at the results of your blood test that may indicate whether you have any kind of lung infection. Otherwise, based on your symptoms your doctor might recommend the following lung function tests for you, as explained by Dr Arya.
'If any of the above mentioned symptoms persist for a long time, it is better to consult a doctor immediately for diagnosis,' says Dr Arya. The management of lung disease depends on the type of lung disease you're diagnosed with but largely medication is the main treatment option for lung disease patients.
Lung Disease: Facts You Need To Know
In August 2019, Angie Abad went to the ER to be treated for a respiratory infection. Medical workers there tested her and prescribed meds, but Abad "never really felt right after that."
After a second respiratory infection and growing problems with breathing, her local hospital still couldn't put a finger on the problem. Finally, a more specialized hospital nearby ran more breathing and lung tests and diagnosed her with the lung disease COPD.
But the diagnosis and the treatments that followed -- including extra oxygen, a nebulizer, and an inhaler -- still left Abad, who is 50 and lives in Denver, without answers to mounting questions. She felt even worse about her condition because she'd watched her father die of the same disease 8 years before.
"I didn't know any questions to ask my pulmonologist," Abad says. "I've just taken the meds she's put me on and left it at that. No one has told me what to expect, possible side effects of meds, or [other] things I would experience."
She didn't find much more support from friends, either. "When you tell people about your diagnosis of COPD, they say, 'Oh,'" she says. "There isn't enough awareness. People don't understand the daily struggles of this disease."
David Mannino, MD, a pulmonologist in Lexington, KY, and the medical director and co-founder of the COPD Foundation, agrees that too many people with lung disease remain in the dark after diagnosis.
On top of people not knowing what questions to ask, "One of the challenges we always seem to have is, a lot of people think it's some type of death sentence. It's not," he says. Mannino has been treating some COPD patients for 15 to 20 years.
Another factor is people with COPD perhaps not knowing they can seek -- and deserve -- support. "A lot of people go into it with shame and blame," Mannino says. For example, smokers might react to their diagnosis by realizing their habit helped set the stage to get the disease. But the guilt should stop there.
"You are dealing with something that is incredibly addicting," Mannino says. "And it's not that way by accident," he says, referring to tobacco companies' longtime knowledge of the harms the substance causes. Even if you can trace the cause of COPD to your lifestyle, this is a time to be gentle on yourself.
Abad filled the many gaps in her grasp of her medical condition "through research, COPD groups, and personal experience."
Her journey has turned up many points she feels are key for people with lung disease to cover with their doctors, answers she wished she'd had all along. They include:
A special question for her was if altitude makes COPD worse. She's newly moved to Denver, which clocks in at 1 mile above sea level. A higher altitude can tax your breathing, mainly at first.
Mannino says he often hears people who have moderate to severe COPD say they wished they'd gone to a pulmonary rehab center or other educational program years before. In these programs, people learn earlier rather than later how to, for example, stretch and breathe properly. They're also taught to fend off panic attacks and times when they can't catch their breath with methods like pursed lip breathing. It's a technique in which you inhale through your nose and breathe out through puckered lips.
Some exercises can actually be fun, Mannino notes, such as playing the harmonica. The higher notes provide ideal breathing workouts.
Such programs also teach people with lung disease how to use meds and lung devices the right way. "Patients learn too late that different respiratory meds require different techniques as to how to use them correctly," Mannino says. "Even physicians might not know how to use these correctly."
However, "the number of rehab programs for COPD are far too few," especially in rural places, he says. The COVID-19 pandemic and its limits on people getting together for anything "nonessential" has made it even harder to get into these programs. Doctors also expect some people who've had COVID will need pulmonary rehab, which will put more strain on the system.
Technology has made it simple for anyone to access disease support, though. A number of lung disease management apps have sprung up, including a free app through the COPD Foundation called the COPD Pocket Consultant Guide. It's designed for people with the disease and their families. You can download it from the foundation website or Google Play.
The app includes links for the right way to use meds, easy ways to track your schedules, and other useful tools rehab programs cover. "You can even print out [info] sheets to give the doctor" to prompt helpful questions and start talks that can sharpen your insights into your condition, Mannino says.
What Are COPD Lung Sounds?
If you have COPD, the sounds made by your lungs can help your doctor evaluate the state of your airways and whether your treatment is working. Types of COPD lung sounds include wheezing, crackling, and ronchi.
COPD refers to a group of progressive lung diseases that make it harder for you to breathe.
Keep reading to understand more about what your healthcare team is listening for when it comes to lung sounds if you're living with COPD.
Your lungs and lung cavity are covered by thin membranes called pleurae. Typically, they slide smoothly over each other to regulate your breathing.
A pleural friction rub is a quick, explosive sound. It can be heard when you breathe in or out. It's a sign that something is interrupting the movement of the membranes.
In COPD, this sound is often due to inflammation.
Wheezing is a high pitched whistling sound. If a healthcare professional hears wheezes in only one area of your lungs, it may be due to a blockage.
In COPD, however, wheezes are more likely to be heard throughout both of your lungs and may be heard throughout the chest
The inflammation that comes with COPD can cause both your large and small airways to narrow. A wheezing sound is the vibration of air through these narrowed airways.
This wheezing sound can sometimes be heard when you breathe in. In most cases, though, it's louder when you breathe out.
Crackles, previously called rales, refer to a noise that's:
A healthcare professional can listen to this sound using a stethoscope, and it's most likely to be heard when you breathe in.
Crackling happens when small air bubbles pass through fluid, which is common in COPD. This can indicate a buildup of mucus or pus in your airways. Coughing temporarily dislodges the fluid, and the crackles go away.
Doctors categorize crackles into three different types:
Stridor is similar to wheezing, but the sound is typically louder than a wheeze. Doctors may hear it when you breathe in or out, and it can indicate upper airway blockages or narrowing.
If stridor is heard when you breathe in, it means there's a narrowing or blockage above your voice box, called the larynx.
If the sound is heard when you breathe out, it means there's a narrowing in your trachea or windpipe. The trachea is the tube that connects your throat to your lungs.
A rhonchus is a continuous sound that may be heard in the lungs. It's a lower pitched sound than a wheeze. Through a stethoscope, it sounds similar to snoring.
This can indicate a buildup of fluid in the larger airways. In COPD, rhonchi can mean the airways are secreting an increased amount of fluids.
Hamman's sign is a crackling or crunching sound that occurs at the same time as your heartbeat. It happens when air gets trapped in the space between your lungs, called the mediastinum.
Air doesn't typically leak into this area. If your doctor detects Hamman's sign, it means there's been damage to your lungs or windpipe, which is causing air to escape.
A whooping sound can happen with coughing when a person is gasping for air. It's the high pitched sound of air rushing into your airways.
This sound is often heard in pertussis, also known as whooping cough. Pertussis is caused by a bacteria.
People with COPD are at greater risk of contracting pertussis. Pertussis can cause COPD symptoms to flare.
Many people are successfully protected from pertussis with vaccination. Talk with your doctor to make sure your immunizations are up to date.
A healthcare professional can hear lung sounds with a stethoscope. Some can be detected even without a stethoscope.
To investigate further, your healthcare team might call for the following tests:
Treatments are available to manage the signs and symptoms of COPD. These include:
Typically, people with stage 1 COPD can have few symptoms, if any, while still displaying a forced expiratory volume (FEV1) between 80-100% of your predicted value. FEV1 is how much air you can expel from your lungs in 1 second.
Can lungs heal from COPD?Once COPD damages your lungs, they cannot return to healthy function. That said, treatments can help your lungs function better and can help you manage your symptoms.
Can people with COPD have clear lung sounds?When your COPD is well-managed or when your symptoms are mild-to-moderate, you're less likely to have atypical lung sounds. In most cases, your lungs will sound clear. If you're experiencing wheezing, it is usually caused by exacerbating factors that can be treated.
Listening to your lungs and airways can provide your doctor with a lot of information about what's going on inside your body.
Certain sounds can indicate narrowing in your airways or fluid buildup. Your healthcare team may require further testing to find out more.




Comments
Post a Comment