Living With Stage 4 Lung Cancer: Survival Rates, Treatments, Emotional Support, and More
I Thought I Pulled A Muscle But I Actually Had Stage 4 Lung Cancer Aged 37 Despite Never Smoking - Here Are The Signs You MUSN'T Ignore
A Texas woman was diagnosed with stage 4 lung cancer at just 37 years old, despite never smoking.
Tiffany Job, a nurse and mother of eight-year-old twin boys, assumed that the pain in her right rib that began in March 2020 was a pulled muscle resulting from a workout.
However, scans would later reveal tumors in her lungs that had spread to her neck, and bones.
'I think I was just in denial, like "This is not happening."' said Tiffany. 'It was shock. A lot of shock.'
Her case comes amid a mysterious rise of cancer cases in people under 40, including colon and appendix cancer.
Lung cancer - the deadliest form of the disease - is also rising, particularly in women, thought to be linked to the fact women are slower to give up cigarettes.
Tiffany Job, 40, was diagnosed with stage four lung cancer after mistaking her symptoms for a pulled muscle
Ms Job's cancer had spread to her pelvis, right femur, and cervical spine
Tiffany's 'pulled muscle' quickly became the least of her problems when a collection of other symptoms cropped up.
On a hiking trip in July 2020, she could barely walk a few feet without her heart rate shooting up and becoming short of breath.
Then, a month later, Tiffany developed a cough that wouldn't subside. Doctors performed blood tests and prescribed a course of antibiotics and steroids.
However, nothing helped.
In September, Tiffany went to her primary care doctor, who ordered a pulmonary function test (PFT). This test measures lung volume and capacity, as well as how air moves through them. 'I failed that miserably,' she told The Patient Story.
Her husband, Nick, said: 'I think they said she had the lung capacity of an 80-year-old.'
'That raised some pretty significant concerns. That was, I think, the first real alarm bell for the primary care doctor.'
'Nobody ever speculated that lung cancer could have even been an option.'
Over the next few weeks, doctors speculated that it could be anything from sarcoidosis - an inflammatory condition caused by an immune overreaction - to Covid to tuberculosis.
Finally, after spending days in isolation, scans revealed that Tiffany had stage four non-small cell lung cancer, which had spread to her pelvis, right femur, and neck.
Ms Job said she was 'in denial' after hearing about the lung cancer diagnosis, especially because she had never smoked
Ms Job posted on Instagram in November that her primary tumor is growing, and her current treatment is ineffective (pictured here with her husband, Nick, and their twin sons)
Lung cancer is the deadliest form of cancer in the US, according to the National Cancer Institute (NCI). It accounts for one in five cancer deaths, followed by colorectal cancer, which causes one in 10 cancer deaths.
About 53 percent of cases are diagnosed when the disease has traveled to multiple other organs.
'The vast majority of lung cancers are diagnosed in the advanced stage because their symptoms don't present until it's moved pretty fast,' Nick said.
The survival rate also drops significantly in these cases, with fewer than 10 percent living for five years.
Only one in four lung cancer patients survive after five years.
There are two main types of lung cancer: small cell and non-small cell.
Non-small cell lung cancer is the most common type, accounting for nine out of 10 lung cancer diagnoses, and typically grows more slowly. It usually doesn't cause any symptoms until it has progressed.
Lung cancer is the deadliest form of cancer in the US, according to the National Cancer Institute (NCI). The survival rate drops sharply as cancer spreads. Advanced lung cancer has just an 8.2 percent five-year survival rate
The above shows lung cancer cases among men and women split by age groups. It reveals the disease is now more common in younger women, compared with other groups
Signs of non-small cell lung cancer, according to the NCI, include chest pain or discomfort, a lingering cough, trouble breathing, wheezing, coughing up blood, loss of appetite, unintentional weight loss, fatigue or lethargy, trouble swallowing, and swelling in the face or veins in the neck.
Cigarette smoking is the leading cause of lung cancer, though Tiffany noted that she never smoked. Exposure to secondhand smoke has also been shown to increase this risk.
Men were nearly twice as likely as women to develop the disease in the 1980s, driven by higher smoking rates and workplace exposure to substances like asbestos.
But with declining cigarette use and increased safety regulations, the pattern has flipped, with young and middle-aged women now being diagnosed with the disease at higher rates than men.
Some evidence suggests this is because women are slower to quit smoking.
Tiffany's tumor had a genetic mutation known as EGFR (epidermal growth factor receptor). This means the cancer causes an excess of the EGFR protein, which can accelerate the growth of lung cancer cells.
This qualified her for a clinical trial of a drug that would specifically target the mutation.
'The prognosis for lung cancer is pretty bad, and chemo doesn't have a good track record, especially for her subtype of cancer,' Nick said.
Tiffany added: 'When we heard "clinical trial," I was very open to it. I think being a nurse, I've always been pretty open to things like that.'
'I feel like that's how we learn. We don't get information if people don't do it.'
However, Tiffany posted on Instagram in November that, despite the novel therapy, the primary tumor in her lung is growing, and her current treatments are no longer effective.
Still, she remains optimistic.
'We don't know what's going to happen to us by the end of the day, so we may as well just live for each and every moment,' she said.
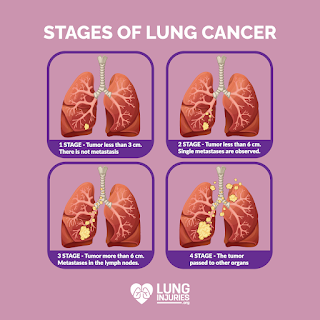
Four Stages Of Cancer And What Each One Means - From 'non-invasive' To Terminal
The dreaded C word is no longer the death sentence it used to be - especially if the disease is caught early. Doctors use a stage system from 0-4 to identify the size of the tumours and whether the cancer has spread
There are more than 200 different types of cancer (Stock photo) (Image: Getty Images/iStockphoto)
In the UK, one in two people will develop some kind of cancer during their lifetime.
But the dreaded C word is no longer the death sentence it used to be, especially if detected early. In fact, cancer survival in the UK has doubled in the last 50 years - and easier to treat variants such as testicular cancer have a 98 per cent survival rate.
Surgery is usually the first treatment people try as solid tumours can be surgically removed. Other methods include chemotherapy and radiotherapy. But, what exactly are the four stages of cancer and what does each one mean?
The NHS says cancer can be categorised using different methods. The TNM staging system uses a variety of letters and numbers to describe the state of the condition, including how big tumours are and whether the cancer has spread. Doctors will also use a staging system from 0-4.
Stage 0: The cancer is where it started and has not spread.
Stage 1: The cancer is small and hasn't spread anywhere else
Stage 2: The cancer has grown but has not spread
Stage 3: The cancer is larger and may have spread to surrounding tissue. May have also spread to the lymph nodes or 'glands'
Stage 4: The cancer will have spread from where it started in the body to at least one other organ. This is also referred to as 'secondary' or 'metastatic' cancer.
Want the latest health news and fitness tips sent straight to your inbox? Sign up to our Health Newsletter
Stage zero, otherwise known as Carcinoma in situ, means that there is a group of 'abnormal cells in area of the body' - but that these are too small to form a tumour. According to Cancer Research, some experts refer to this these cell changes as 'non-invasive cancer' or 'precancerous changes'. This doesn't mean that treatment itself won't be invasive - as surgery and radiotherapy are still commonly used at this stage.
When a person's cancer is not curable and will result in death, doctors use the term 'terminal'. However, this is not linked to a specific stage. Even those diagnosed with stage four cancers are not always terminal - and may just require more aggressive forms of treatment.
Survival ratesIt makes sense that the earlier the stage of cancer - the better the survival rates - but this does vary depending on which variant of the disease we're talking about. According to the Office for National Statistics : "Apart from lung and ovarian cancer, there is a pattern of similar one year survival for patients diagnosed at stages 1 - 3 and a large decrease for those diagnosed at stage 4".
The stage four survival rate varies from 15 per cent (men with lung cancer) to 83 per cent (men with prostate cancer) - showing again that stage four cancer does not mean 'terminal' . The low figure for lung cancer could be attributed to the fact that many cancers are diagnosed much later on in comparison to others.
Colorectal cancer's one year survival is similar for men and women at all stages. Whereas ovarian cancer's one year survival rates steadily decreases with increasing stage, meaning an early diagnosis is essential.
There are many early warning signs of cancer, including finding a lump that suddenly appears on your body, unexplained bleeding, and changes to your bowel habits. It's important to see a GP if you're worried about your symptoms.
Do you have a story to share? Email us at yourmirror@mirror.Co.Uk
For Cancer Patients, Clinical Trials Can Come With Significant Out-of-pocket Costs
NEW ORLEANS — Every three weeks, Shenard Matthews makes the sign of the cross and prays before he jumps into his truck for a five-hour drive to Houston.
For more than a year, the 53-year-old, who lives with stage 4 lung cancer, has been making this trip to get life-saving care not offered in his home state.
Earlier this month, he left at two in the morning to avoid traffic for his next round of treatment and tests at the MD Anderson Cancer Center, which has an extensive cancer clinical trials program.
Tumors have damaged his spine and neck, which makes it a long, painful drive. His 11-year-old truck is in bad shape, too. It has close to 200,000 miles; the engine runs loud during the hourslong drive.
"If I get a flat, I can't change it. I don't have the strength anymore," Matthews said. He worries about his truck breaking down or getting too sick to drive. "I have no other transportation. It's very stressful, and I'm not in the best shape, but it's my only hope."
Clinical trials are studies that help doctors and researchers find better ways to care for people with cancer and give patients access to the latest therapies. Cancer clinical trials can offer hope for cancer patients with late-stage disease or for whom conventional treatments fail. Each year, more than 25,000 Louisianans receive a new cancer diagnosis. But many, like Matthews, don't have access to new trials and therapies near their home.

Shenard Matthews sits in a chair at MD Anderson Cancer Center in Houston, getting treatment for stage 4 lung cancer. Each month, he's had to travel hundreds of miles away from home to participate in a clinical cancer trial not offered in Louisiana. In the right photo, he celebrates with nurses after seeing a major reduction in tumor size, which is extending his life. Photo courtesy of Matthews family
Fewer than 5 percent of adult patients with cancer enroll in a clinical trial, according to a 2019 study by the American Society of Clinical Oncology. Many must seek out treatments that may be far away, creating financial burdens due to the high cost of travel. These challenges can pose a "significant and sometimes insurmountable barrier," according to the American Cancer Society.
The state has the sixth worst rate of new cancers, as well as the seventh highest cancer death rate in the country. Residents continue to get sick from and die from cancer more often than in most other states, while health disparities in mortality persist, according to Louisiana's Comprehensive Cancer Control Plan released last March. White patients in the state have a higher survival rate than those who are Black, the plan says. The risk for lung cancer, for example, is 58 percent higher for Black men than white men.
The pandemic didn't help. A 2023 study published in Lancet Oncology found a "substantial" drop in early-stage cancer diagnoses during the first year of the COVID-19 pandemic. The disruptions to care caused by the pandemic meant patients were most likely to receive late-stage cancer diagnoses, disproportionately affecting rural areas and communities of color.
Matthews, who is Black, lives in a rural community located in an area known as "Cancer Alley." The pollution from petrochemical production in the industrial plants that dot this 85-mile stretch along the Mississippi River has been linked to elevated cancer risks and rates.
Matthews worked at a chemical plant for 15 years. Looking back, he said he didn't get the care he needed, although he regularly had physicals. A chest X-ray for pneumonia in 2021 failed to detect cancer. Then, a subsequent X-ray for a hernia revealed a spot on his lungs. He said once he was officially diagnosed in 2022, his doctor never mentioned one thing that could help him — a clinical trial.
"The doctor said, 'Unfortunately, Mr. Matthews, you don't have that much time left, and there's not much we can do about it.' He was giving me like four months," the father of four said. "I just fell apart. I never felt like that in my life."
On his own, Matthews found another option: high-quality cancer care and advanced treatments by way of a clinical trial — 350 miles away in Houston. Even then, insurance coverage for the procedure was denied twice because of the "high risk." Matthews persisted and self-advocated his way into the trial. But he still incurred out-of-pocket costs for gas, hotel stays, parking, tolls, vehicle wear and tear, companion costs, and other items he couldn't afford because he lost his job.
"It got so bad, I was taking a Greyhound bus, the cheapest that you can go."
Matthews said his community in Lutcher, Louisiana, has rallied with fundraisers, but it has faded over time. He moved in with his mother to continue treatment and save money. He now travels alone without someone to help him with the side effects of the treatments.
"I'm very grateful for what my community did for me already. I'm that type of man that is not gonna go door-to-door for a handout, but having cancer doesn't help, especially when I have a daughter in college," Matthews said. "I still have to be a father. I have a car note. I have car insurance. I have to make sure my truck is in good shape so I can go back and forth to Houston."
But the bills keep adding up. "I try not to think of it. It got so bad, I was taking a Greyhound bus, the cheapest that you can go," he said.
READ MORE: EPA drops environmental justice investigations in Louisiana
Patients with fewer financial resources may find the indirect or "hidden" costs of trial participation — such as travel, time off work, or daycare needs — prohibitive. Participants in clinical trials pay an average of $600 in indirect costs per month, or $7,200 a year, according to one report from the American Cancer Society's Cancer Action Network (ACS CAN).
For the last 18 years, the California-based nonprofit Lazarex Cancer Foundation has been working to improve access to cancer clinical trials by providing financial reimbursement for travel costs associated with participating in the research. Lazarex has seen an explosion of need. What began as helping three patients in 2006 has grown to assist more than 2,000 patients last year. On average, patients the foundation has helped have traveled an average of 544 miles to get to their cancer clinical trials.
The foundation, citing budgetary restraints, has not accepted new clients since October. The nonprofit said the process could resume in April.
Matthews is one of the patients who turned to the nonprofit for help in funding his trips and continuing his care. His tumors have reduced, and his cancer cells have become dormant, he said, which is extending his life.
Lazarex CEO and founder Dana Dornsife said cancer clinical trials can be a lifeline. "When you are experiencing financial toxicity from a cancer diagnosis, every cent becomes a consideration for a patient, and all too often, it's the barrier that prevents patients from being able to say, 'Yes, I want to participate.' I know beyond a shadow of a doubt that it's costing lives."
Dornsife started the nonprofit after her family experienced the same challenges when her brother-in-law was diagnosed with pancreatic cancer. He needed help finding a clinical trial and was burdened by the cost of care.
"It is shocking to me, we still have all of these patients out there who need this assistance, and they're not even going to be able to walk out their front door to go to a clinical trial if they don't get this financial assistance for travel reimbursement," Dornsife said.
The Cancer Society of Louisiana says options for travel reimbursement are non-existent despite a significant need for out-of-town access to clinical trials. Most of the available grants are restricted to in-state patients only, and funds are limited. Last year, the group spent nearly $90,000 on gas cards and food assistance.
"It is a void, but we can only do so much," said Tammy Swindle, executive director for the Cancer Association of Louisiana. "Our two biggest things that we get requests for are transportation and food. We can't reimburse patients directly. I hate to turn people down, but we can't do huge things like hotels or airfare. We just don't have money for that, even though clinical trials are the things that help a lot of people. Sometimes it's their last hope."
Swindle said the money goes quickly, and it's not enough. What she can do is give out gift cards and provide utility and rental assistance, which frees up household money for patients to use for travel expenses.
"I think more people should be talking about it because they need people to go into clinical trials for them to succeed," Swindle said. "If one of the barriers is transportation to get there or housing to stay, they [research funders] should help with that."
WATCH: What to know about screening, diagnosis and treatment for prostate cancer
As many as one out of five cancer clinical trials fail to enroll enough patients due to lack of participation, the ACS CAN report found. This matters because low participation rates can cause a trial to stall or fail, and precious time and resources that could advance cancer research are wasted, according to a 2018 landscape report from the ACS CAN.
The group has tried for the last two years to introduce legislation that allows clinical trial sponsors to financially support patients without creating a conflict of interest and help prevent fraud abuse.
"The patient should not suffer financially anymore. They have suffered enough with the disease itself."
"We know that those of lower income are very sensitive to any added cost that they perceive might be involved in a clinical trial. We also know that sponsors are willing to support patients who need this and want this," said Mark Fleury, the group's policy principal on emerging science and leader of its clinical trials portfolio. "We want to try and clear the deck of any unnecessary hurdles to make that possible. There's only so much foundation and philanthropic money out there to support folks. This legislation would create a safe harbor for financial support for nominal costs.
Citing a 2021 survey, the network said that nearly 80 percent of cancer patients said they were more likely to join clinical trials if the sponsors behind the research studies helped offset travel costs.
"We need to wake up, and we need to get real about it. We need to start including these types of expenses as part of a treatment trial," Dornsife said. "The patient should not suffer financially anymore. They have suffered enough with the disease itself."
Dornsife said that beyond making patients whole, diverse participation has a tremendous effect on the trials to reduce biases.
Louisiana's leaders are aware of the suffering caused by cancer but have struggled to make progress on bringing more trials to the state. More than 9,300 Louisianans die from cancer each year. The mortality rate is also costly to the state's economy, with estimated productivity losses of about $400 million each year due to excessive early death.
The state launched a renewed commitment last November with four top research institutions to accelerate its effort to secure a National Cancer Institute (NCI) designation that has eluded the state for more than two decades.
LSU Health, LCMC Health, Tulane University, and the Louisiana Cancer Research Center, which have often collaborated even as they compete for patients and research dollars, have agreed to formalize their work under one umbrella. An NCI designation means support from the federal agency, including advanced research and funding, cutting-edge cancer treatments, and training and support for cancer researchers.

Louisiana has among the highest cancer rates in the nation. State leaders announced a new strategy in November to renew a two-decade-long effort to get the state's first National Cancer Institute designation. Photo courtesy of Louisiana Cancer Research Institute
Gov. John Bel Edwards said at the time the NCI designation would have a "profound impact" on the state, allowing "vulnerable populations in Louisiana who may not have the means to travel to get care much closer to home."
There are 72 NCI-designated cancer centers in 36 states and the District of Columbia that are funded by the institute. A 2009 Dartmouth study suggested that patients who receive care at an NCI-designated cancer center can improve their long-term survival rates by up to 25 percent.
Dr. Joe Ramos, the director and CEO of the Louisiana Cancer Research Center who leads the state's research efforts, says it could take six years for the state to submit an application for the designation and another year for it to be approved. Still, the state-level collaboration is a breakthrough, he said.
"It's an all-hands-on-deck kind of moment if we're going to make a difference. In almost every health metric, Louisiana is at the very bottom," Ramos said. "This is a state that is in dire need of a reduction in the burden of cancer that we sustain here."
Ramos said there is a lot of "good basic bench research and some amazing community outreach but a real lack of coordination." A multi-tiered approach is needed, he said.
"We have the challenges of having the right programs in place for the clinical trials, the right programs for community education, and having our communities work to help themselves with our help," Ramos said. "It's not just something that the cancer center will be able to do itself. We've got to work with our advocates, with the stakeholders across the state to help make sure there are better outcomes. It is an enormous challenge, and that's why it's been so difficult to dent it."
An NCI-designated cancer center could prevent about 6,550 deaths over 10 years, according to a 2003 paper in the Journal of the Louisiana State Medical Society. There would also be potential revenue generated through new patients from neighboring states, diversion of Louisiana patients back to the state from other out-of-state facilities, and the indirect benefits derived through increased economic productivity. Every one million dollars spent could bring about $8.5 million worth of economic benefits, according to the analysis.
"It is a big hill to climb. We've got to start to show this cancer center is having an impact in measurable ways," Ramos said. "It's only going to be when we show that we're helping solve some of the problems that we have any chance of getting this NCI designation."
For Matthews, it's unclear whether an NCI-designated cancer center will help. He's been told his non-small cell lung cancer is incurable.
For now, the cancer trial has helped shrink the tumors and prolong his life, but it comes with a lot of stress. He's unsure what is worse: the disease, the financial strain, or both.
"It has meant so many hardships piled on so many hardships," Matthews said as he choked up and paused. "It's very hard to be happy about getting the treatment. What's hard about it is you don't know if you gonna wake up the next day. Still, I'm going to give it all I can give it."




Comments
Post a Comment